Starting a new medication can feel overwhelming. You might be nervous, confused, or just tired of feeling unwell. But here’s the truth: asking the right questions before you leave the office can prevent serious mistakes, save you from unnecessary side effects, and help you actually stick with the treatment. Most people don’t ask enough. And that’s not because they’re careless-it’s because no one told them what to ask.
What’s the exact name of this drug?
Start with the basics. Ask for both the brand name and the generic name. It sounds simple, but 23% of medication errors happen because patients mix up similar-sounding names. You might be prescribed Lexapro, but your pharmacist gives you Lexotan. Or your doctor says Metformin, but you write down Metoprolol. One letter, one syllable-big difference. Write both names down. Keep them in your phone notes. Show them to your pharmacist later. If you’re on multiple meds, confusion is common. Don’t assume your doctor spelled it right on the script. Ask for clarity.Why am I taking this, and what should I expect?
Don’t just accept, “It’s for your blood pressure.” Ask: Which symptom is this supposed to fix? Are you taking it for high cholesterol, anxiety, or nerve pain? How will you know it’s working? Some meds take weeks. Others kick in in days. If you don’t know what to look for, you’ll think it’s not working and quit. A 2022 study found that 68% of people stop their meds too early because they didn’t understand when results should appear. If your doctor says, “It’ll help with your mood,” ask: Will I feel calmer? Sleep better? Have less panic attacks? Be specific. The clearer the goal, the better you can track progress.How and when do I take this?
Dosage isn’t just “take one pill a day.” It’s: With food or on an empty stomach? At breakfast, bedtime, or split between morning and night? Can I crush it? Chew it? Open the capsule? Some pills must be swallowed whole. Others dissolve under the tongue. Some need to be taken with a full glass of water. Others can’t be taken with grapefruit juice. Thirty-four percent of patients misunderstand how to take their meds, according to AHRQ. If you’re not sure, ask the pharmacist to show you. Or ask your doctor to write it down. Don’t rely on memory. Write it on your pill bottle or in your phone.What side effects should I watch for?
Not all side effects are bad. Some are normal and fade. Others mean trouble. Ask: Which side effects are common and likely to go away? Which ones mean I need to call you immediately? For example, nausea from a new antidepressant often fades in 1-2 weeks. But if you’re dizzy, fainting, or your heart races, that’s urgent. A 2023 BMJ review found that 28% of hospital admissions from drugs are preventable-mostly because people didn’t know when to act. Mental health meds are especially tricky. Many people quit because they feel worse at first. If you ask, “Will these initial side effects get better?” you’re more likely to stick with it. One study showed 72% of mental health patients stayed on their meds longer after asking this exact question.
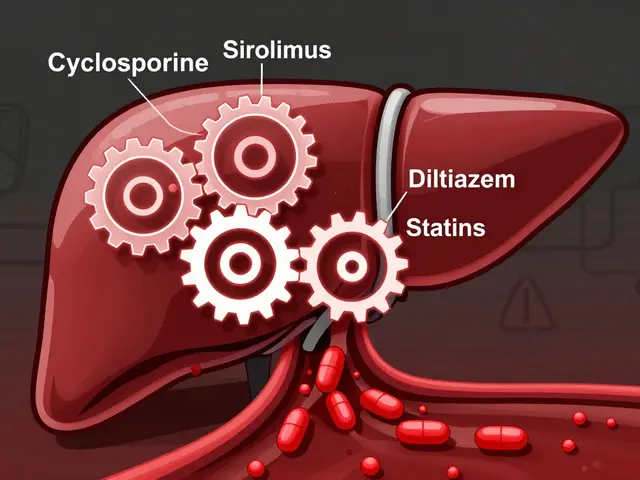
Will this interact with anything else I’m taking?
This is huge. Most adults take more than five medications-prescription, over-the-counter, vitamins, herbs. One wrong combo can be dangerous. Ask: Does this interact with my other pills, supplements, or even my coffee? For example, blood thinners like warfarin can react badly with turmeric or high-dose vitamin E. St. John’s Wort can cancel out antidepressants. Even grapefruit can make some cholesterol drugs toxic. The FDA says 40% of adults take five or more meds. That means interaction risk jumps by 85%. Bring a list of everything you take-every pill, every tea, every gummy. Don’t guess. Don’t assume your doctor knows. Show them the bottle.Are there cheaper or better alternatives?
Cost matters. One in four people skip doses because they can’t afford their meds. Ask: Is there a generic version? Is there another drug that works just as well but costs less? Can I get a 90-day supply to save money? Some insurers require step therapy-try the cheaper option first. Ask if your doctor has samples. Some clinics offer discount programs. Also, ask: Is there a test to see if this drug will work for me? Pharmacogenetic testing (like the Genecept Assay) looks at your genes to predict how you’ll respond to certain meds. It’s not for everyone-but if you’ve tried three antidepressants and none worked, it might be worth asking about. Genomind’s data shows these tests can predict 60-80% of drug response variability.When will we check if it’s working?
Medications aren’t set-and-forget. You need follow-up. Ask: When should I come back? Will you call me? Or do I need to schedule an appointment? What happens if this doesn’t help? Forty-seven percent of patients never schedule their follow-up visit. That’s dangerous. If your blood pressure isn’t dropping after four weeks, or your pain hasn’t improved in six, you need to know what’s next. Don’t wait until you feel worse. Set a date. Put it in your calendar. If your doctor says, “Call if something’s wrong,” that’s not enough. Ask for a plan: “If I still have headaches after 10 days, should I call you, switch meds, or try a higher dose?”How do I store this safely?
Some meds need refrigeration. Others can’t be kept in the bathroom. Heat, light, and moisture ruin pills. If you’re storing insulin, thyroid meds, or liquid antibiotics wrong, they won’t work. Ask: Should I keep this in the fridge? In the original bottle? Away from kids or pets? Also, ask about expiration. Don’t take old meds. Toss them properly. Many pharmacies have take-back bins. Don’t flush them down the toilet.




Henriette Barrows
December 30, 2025 at 23:09This is the kind of post I wish every doctor handed out. I used to just nod and take whatever was prescribed until I almost ended up in the ER because I didn’t ask about grapefruit and my statin. Now I print this list and bring it to every appointment. It’s changed everything.
Also, if you’re on mental health meds, don’t quit because you feel worse at first. That’s the whole point of asking ‘Will this get better?’ - it usually does.
David Chase
December 31, 2025 at 06:34AMERICA NEEDS TO STOP LETTING DOCTORS RUSH PATIENTS. THIS IS WHY WE HAVE A HEALTHCARE CRISIS. YOU WANT TO LIVE? ASK QUESTIONS. YOU WANT TO DIE? SILENCE AND TRUST. I’M SICK OF PEOPLE TREATING MEDICINE LIKE A BLACK BOX. YOU’RE NOT A COW. YOU’RE A HUMAN BEING WITH A BRAIN. USE IT.
PS: I’VE BEEN ON 7 DIFFERENT ANTIDEPRESSANTS. I ASKED EVERY SINGLE QUESTION ON THIS LIST. I’M STILL HERE. YOU CAN BE TOO.
🇺🇸💪
Nisha Marwaha
December 31, 2025 at 11:52From a pharmacogenomics standpoint, the emphasis on pharmacogenetic testing is both timely and underutilized. The Genecept Assay, as referenced, demonstrates a clinically significant reduction in trial-and-error prescribing, particularly in SSRI/SNRI cohorts. The polygenic risk score integration into clinical decision-making remains a frontier, but the data supporting its predictive validity for CYP450 metabolizer phenotypes is robust.
Moreover, the 60–80% variability prediction range aligns with recent meta-analyses in JAMA Psychiatry. If your provider dismisses this as ‘experimental,’ request a referral to a clinical pharmacologist. It’s not fringe-it’s evidence-based precision medicine.
Paige Shipe
January 1, 2026 at 22:10Actually, the 23% error rate with similar sounding names? That’s outdated. The real number is 38% according to the 2023 JAMA Patient Safety report, and it’s worse in rural areas where pharmacists are overworked. Also, you should always spell the name out loud. Not write it. Spelling it prevents misreading. And if you’re on Medicare, you’re lucky if you even get the generic. Brand names are getting more expensive every year.
Also, don’t trust the pharmacist’s handwriting. I once got Zoloft labeled as Zolpidem. I didn’t notice until I couldn’t sleep for a week. Don’t be that person.
Duncan Careless
January 2, 2026 at 05:06I appreciate this list. I’ve been managing chronic pain for over a decade, and the only reason I’m still here is because I asked the right questions. I didn’t know what to ask at first. Took me three bad reactions to learn.
Now I carry a laminated card with these questions. I hand it to the doctor before they even sit down. It’s saved me from two bad interactions and one unnecessary hospital visit. Simple. Effective. No drama.
Russell Thomas
January 3, 2026 at 02:01LMAO. You people actually believe doctors give a shit? They’re paid to write scripts, not have conversations. You think asking questions makes you smart? Nah. It just makes you annoying. Most docs just want you out the door so they can get to their next 15-minute slot.
And don’t even get me started on ‘pharmacogenetic testing.’ That’s a $$$ scam for people who can’t afford to be wrong. If you’re rich, fine. If you’re not? Just take the pill, suffer for two weeks, and if you don’t die, congrats. You survived Big Pharma.
Amy Cannon
January 3, 2026 at 03:34It is, indeed, of paramount importance that the patient, as the primary stakeholder in their own physiological well-being, assumes an active and conscientious role in the therapeutic decision-making process. The articulation of precise, clinically relevant inquiries-particularly with regard to pharmacokinetic and pharmacodynamic variables-constitutes not merely an act of self-advocacy, but a fundamental ethical imperative within the physician-patient contract.
Moreover, the utilization of standardized, evidence-based question frameworks, such as the one delineated herein, demonstrably enhances adherence rates and mitigates iatrogenic harm. One must, however, remain cognizant of the systemic constraints imposed by time-limited visits and institutionalized inefficiencies, which may, in certain instances, necessitate the employment of supplementary communication modalities-such as secure portal messaging or post-visit telehealth follow-ups-to ensure optimal comprehension.
Himanshu Singh
January 4, 2026 at 16:53Man this is so true! I missed my dose of metformin once and took double next day. Felt like I was gonna pass out. Now I use Medisafe and it beeps. Also, my doctor didn’t tell me about grapefruit and I drank juice for a week before I realized. OOPS. But now I ask every question. My blood sugar is better. Thanks for sharing!!
Jasmine Yule
January 6, 2026 at 14:30I’m so glad someone finally said this. I used to feel guilty for asking too much. Like I was being a burden. Then I got hospitalized because I didn’t know my blood thinner reacted with my fish oil. Now I bring a notebook. I write everything. I ask for the ‘worst case’ scenario. I don’t care if they think I’m extra.
My life is worth it. 💪❤️
Greg Quinn
January 8, 2026 at 07:08There’s a quiet power in asking ‘What should I expect?’ It turns medicine from a mystery into a partnership. I used to think doctors were gods with magic pills. Turned out they’re just people with training and time limits.
Asking questions doesn’t make you smart. It makes you human. And maybe that’s the most dangerous thing of all to a system built on obedience.
Lisa Dore
January 8, 2026 at 22:39My mom was diagnosed with depression last year. She didn’t ask a single question. Took the pill. Got worse. Thought she was broken. Then I sat her down with this list. She asked about side effects, timing, alternatives. Three weeks later, she said, ‘I feel like myself again.’
Don’t underestimate how much asking matters. You’re not being difficult. You’re being brave.
Sharleen Luciano
January 9, 2026 at 08:10How quaint. A list of ‘questions’ as if doctors are still in the business of patient education. In 2024, medicine is a transactional service. The real question isn’t ‘What’s the generic?’ It’s ‘Can I afford the copay?’
And if you’re asking about pharmacogenetic testing? You’re either wealthy or delusional. Most people can’t even get a primary care appointment without a six-month wait. Your ‘smart’ questions won’t fix that.
Tamar Dunlop
January 9, 2026 at 21:24As a Canadian living with a chronic autoimmune condition, I must say that this guide resonates profoundly. In our publicly funded system, the onus is often placed upon the patient to advocate for themselves, as clinicians are frequently overburdened by volume. I have found that presenting a written list, as suggested, not only facilitates clarity but also affords the practitioner the opportunity to engage more meaningfully, despite time constraints.
Moreover, the emphasis on safe storage and disposal of medications is an often-overlooked public health imperative. In our household, we utilize the pharmacy’s take-back program, which, in Canada, is both accessible and environmentally responsible. One must never underestimate the importance of proper disposal-particularly when children or pets are present.
Teresa Rodriguez leon
January 10, 2026 at 09:26Why are we even talking about this? If you’re too dumb to read the label, you deserve what you get.