Triptan Medication Interaction Checker
Your medications:
Safe Combination
Your medications don't appear to interact dangerously with triptans.
Caution
This combination requires medical supervision. Consult your doctor before taking triptans.
Dangerous Interaction
Triptans are not safe with this combination. Do not take triptans without consulting your doctor immediately.
Triptans are the go-to treatment for many people with moderate to severe migraines. They work fast, often cutting pain in half within two hours. But they’re not magic pills. For every person who gets relief, another might get chest tightness, dizziness, or no help at all. And if you’re on antidepressants or have heart issues, triptans could be dangerous. Understanding how they interact with other drugs and where they fall short isn’t just helpful-it’s essential to avoid harm and get real results.
How Triptans Actually Work
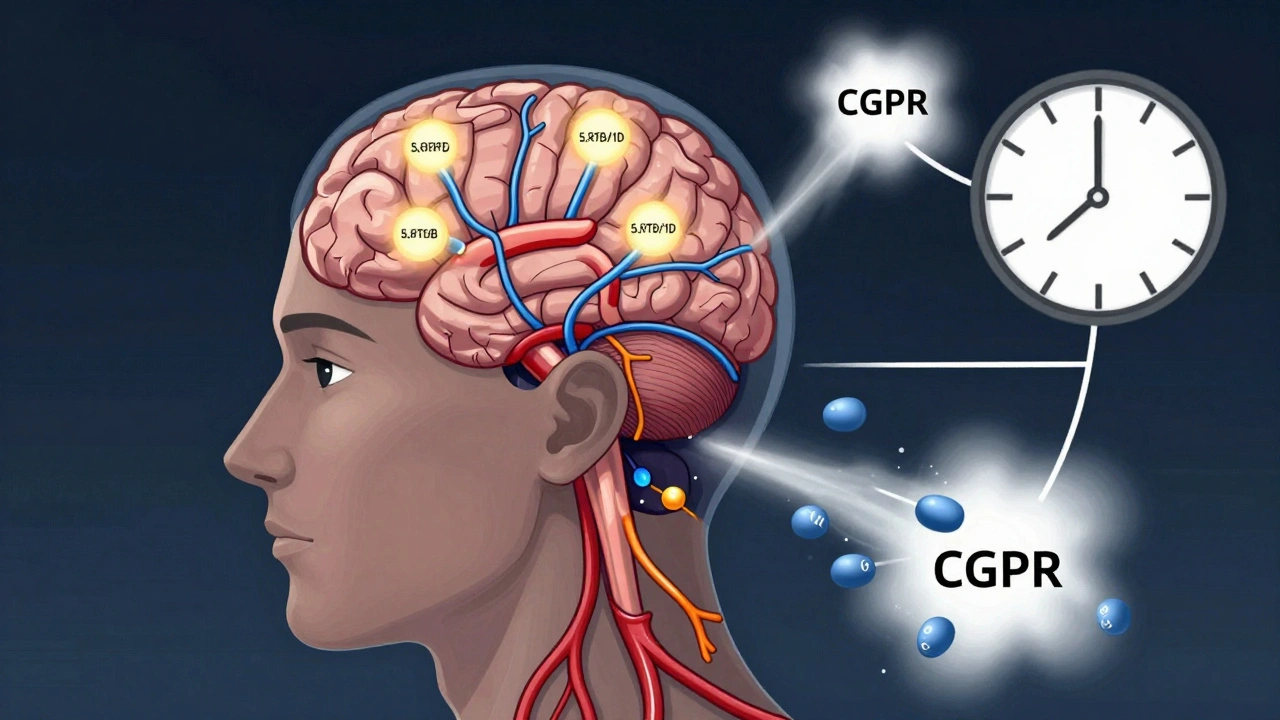
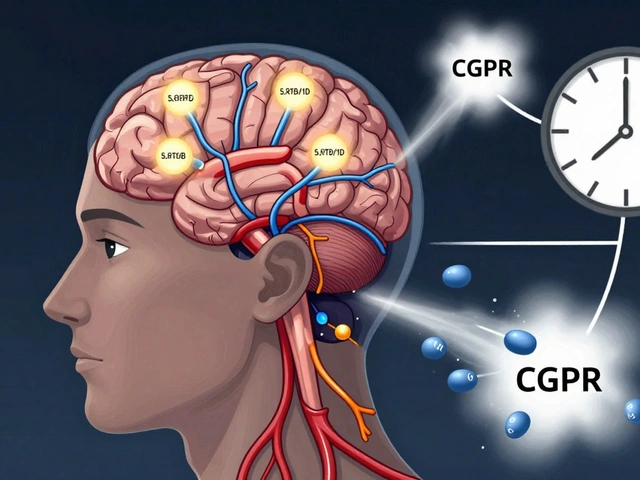
Triptans don’t just mask pain. They target the root of a migraine attack. During a migraine, blood vessels in the brain swell and release inflammatory chemicals like CGRP and substance P. Triptans bind to serotonin receptors-specifically 5-HT1B and 5-HT1D-on nerves and blood vessels. This causes the swollen vessels to tighten and stops the release of those pain-triggering chemicals. It’s why sumatriptan can lower CGRP levels in the blood as the headache fades. This isn’t guesswork; it’s measurable biology.
There are seven FDA-approved triptans: sumatriptan, rizatriptan, zolmitriptan, naratriptan, frovatriptan, almotriptan, and eletriptan. They all end in “-triptan,” but they’re not the same. Rizatriptan and zolmitriptan are absorbed better in the gut, so they work faster. Frovatriptan lasts longer-up to 26 hours-making it useful for migraines that come back. Eletriptan has the highest success rate at two hours (75%), while frovatriptan is the slowest to kick in. Your body’s response depends on which version you take, not just the fact that it’s a triptan.
When Triptans Don’t Work
It’s common to hear, “I tried triptans and they didn’t help.” That’s not just bad luck. About 30% to 40% of migraine sufferers get no relief from any single triptan. And 20% don’t respond to any of them, no matter how many they try. Why? Migraine isn’t one disease-it’s a collection of biological patterns. Genetics, nerve sensitivity, and even how your liver processes drugs can make one triptan useless while another works perfectly.
Timing matters more than most people realize. Taking a triptan too early-during the aura phase-can actually make things worse. Blood vessels are already constricted during aura. Giving a vasoconstrictor then doesn’t help and may even trigger more neurological symptoms. The sweet spot is right when the pain starts. If you wait more than 20 minutes, effectiveness drops sharply. One study found that patients who took their triptan within 20 minutes of pain onset had nearly double the chance of being pain-free at two hours compared to those who waited.
Another big reason triptans fail? Cutaneous allodynia. That’s when your skin becomes painfully sensitive-like brushing your hair or wearing glasses hurts. If you have this, triptans are far less effective. In patients without allodynia, success rates are 70-80%. With it? They drop to 30-40%. This isn’t just discomfort-it’s a sign your nervous system is in overdrive. Triptans can’t calm that level of sensitization.
Dangerous Interactions
Triptans can be risky if you’re taking other drugs that affect serotonin. SSRIs like sertraline or SNRIs like venlafaxine are common antidepressants. Combining them with triptans raises the risk of serotonin syndrome-a rare but serious condition where your body has too much serotonin. Symptoms include confusion, rapid heart rate, high blood pressure, muscle rigidity, and fever. It’s not common, but it’s real. Documented cases are rare, but they happen. If you’re on an antidepressant and your doctor prescribes a triptan, make sure they know exactly what you’re taking.
There’s also the issue of ergotamines and opioids. Both are sometimes used for migraines, but they shouldn’t be mixed with triptans. Using them together increases the risk of severe vasoconstriction, which can lead to heart attack or stroke. Even waiting 24 hours between doses isn’t enough. These combinations are not just discouraged-they’re banned in clinical guidelines.
And don’t forget about MAO inhibitors. If you’re on an MAOI for depression or Parkinson’s, triptans are strictly off-limits. The interaction can cause dangerous spikes in blood pressure and serotonin overload. Always tell your doctor about every medication, supplement, or herbal remedy you use. St. John’s Wort, for example, also affects serotonin and can add to the risk.
Who Should Never Take Triptans
Triptans are not safe for everyone. They’re absolutely contraindicated if you have:
- Ischemic heart disease or a history of heart attack
- Coronary artery spasm (Prinzmetal’s angina)
- Stroke or transient ischemic attack (TIA)
- Uncontrolled high blood pressure
- Peripheral artery disease
- Severe liver damage
Why? Because triptans narrow blood vessels. If your heart or brain arteries are already narrowed by plaque or spasm, further constriction can cut off blood flow. The risk is small-about 0.08 heart attacks per 10,000 patient-years with sumatriptan-but it’s real. And if you’ve had a stroke before, another one could be fatal.
Even if you don’t have a diagnosed condition, if you’re over 40 and have risk factors-smoking, diabetes, high cholesterol, or a family history of heart disease-you need a careful evaluation before using triptans. Your doctor might recommend an ECG or stress test first. Don’t assume you’re fine because you’ve taken them before. Risk changes over time.
Dosing Limits and Overuse
Triptans are powerful, but more isn’t better. Taking more than two doses in 24 hours increases your risk of medication-overuse headache (MOH). That’s when your headaches get worse because you’re using painkillers too often. The International Headache Society says no more than two doses per day, with at least two hours between them. That’s not a suggestion-it’s a hard limit.
Some triptans, like naratriptan and frovatriptan, are longer-acting. People think they can take them more often because they last longer. That’s wrong. The same limits apply. Even if you only take one dose of frovatriptan, you still can’t take another for 24 hours. And if you find yourself using a triptan more than 10 days a month, you’re already in MOH territory. That’s when you need to step back and rethink your treatment plan.
Many people stop taking triptans within a year-not because they work too well, but because they don’t work well enough. Side effects like chest tightness (5-7% of users), dizziness (4-10%), and fatigue (3-8%) are common enough that people quit. Cost is another factor. Brand-name versions can cost $100 or more per pill. Generic sumatriptan is cheaper, but even then, insurance often limits how many you can get per month.
What Comes After Triptans?
Triptans still make up 45% of the acute migraine treatment market. But things are changing. Newer drugs called gepants (like ubrogepant and rimegepant) and ditans (like lasmiditan) don’t constrict blood vessels. That makes them safer for people with heart problems. Gepants block CGRP, the very chemical triptans try to suppress. And they work without the chest pressure or dizziness that turns people off triptans.
For those who don’t respond to triptans, switching between them can help. About 30-40% of people who fail one triptan respond to another. That’s why doctors often recommend trying at least two or three before giving up. It’s not random. Different triptans have slightly different receptor binding patterns. One might work better if your migraine is triggered by a specific nerve pathway.
Combination therapy is another option. Sumatriptan plus naproxen (a common NSAID) works better than either alone. The 2-hour pain-free rate jumps from 18% with sumatriptan alone to nearly 27% with the combo. That’s a big jump for people who need to get back to work or care for kids. And it’s available as a single pill now-Treximet.
For chronic migraine sufferers, preventive treatments like CGRP monoclonal antibodies (e.g., Aimovig, Emgality) are becoming standard. These aren’t for single attacks-they’re monthly shots that reduce how often migraines happen. If you’re using triptans more than four times a month, it’s time to talk about prevention.
What to Do If Triptans Aren’t Working
If you’ve tried one or two triptans and got nothing, don’t assume they’re all useless. Try a different one. Switch from oral to nasal spray or a dissolving tablet-those work faster and bypass stomach absorption issues. Rizatriptan orally disintegrating tablets or zolmitriptan nasal spray often give better early relief.
If you have side effects like chest tightness, ask your doctor about alternatives. Lasmiditan (a ditan) doesn’t constrict blood vessels, so it won’t cause that feeling. Gepants are another option. Both are newer, but they’re FDA-approved and covered by many insurance plans now.
Track your attacks. Note when they start, how long they last, whether you had aura, if you had skin sensitivity, and what you took. That data helps your doctor pick the right next step. Don’t just keep taking the same pill hoping it’ll work better next time.
And if you’ve tried everything and still have no relief? You’re not alone. About 10% of migraine patients don’t respond to any triptan or newer drug. That’s when specialized headache clinics step in. They look at nerve blocks, neuromodulation devices, or even clinical trials. There’s always another path-even if it’s not the one you expected.
Can I take a triptan with my antidepressant?
It depends. Triptans can interact with SSRIs and SNRIs, raising the risk of serotonin syndrome-a rare but serious condition. While documented cases are uncommon, the risk is real. Never combine them without your doctor’s approval. If you’re on an antidepressant and need a triptan, your doctor may choose one with lower interaction potential or adjust your doses. Always list every medication you take, including over-the-counter and herbal supplements.
Why do triptans sometimes make my headache worse?
Triptans can make migraines worse if taken too early-during the aura phase. During aura, blood vessels are already constricted. Giving a vasoconstrictor like a triptan at that point doesn’t help and may trigger more neurological symptoms. Always wait until the pain starts. Taking it at the first sign of headache gives the best results. If you take it during aura, you’re treating the wrong phase.
Are triptans safe if I have high blood pressure?
Only if your blood pressure is controlled. Triptans narrow blood vessels, which can raise blood pressure further. If you have uncontrolled hypertension, triptans are dangerous and strictly avoided. If your blood pressure is managed with medication and stable, your doctor may still prescribe a triptan-but only after evaluating your heart health. Always check your blood pressure before taking one, and never use it if your reading is above 140/90.
How many triptans can I take in a day?
You should never take more than two doses of any triptan in a 24-hour period. Doses must be at least two hours apart. Taking more increases your risk of medication-overuse headache, where your headaches become more frequent and harder to treat. Even long-acting triptans like frovatriptan follow this rule. If you need more than two doses a month, talk to your doctor about preventive treatments instead.
Why do triptans stop working over time?
Triptans don’t usually lose effectiveness because your body builds tolerance. More often, the migraine itself changes-becoming more frequent, longer, or developing new symptoms like skin sensitivity (allodynia). If you’re using triptans more than 10 days a month, you’re at risk for medication-overuse headache. That’s when the medicine starts causing the problem. Switching triptans or adding a preventive treatment can help reset your system.
What are the most common side effects of triptans?
The most common side effects are chest or throat tightness (5-7%), dizziness (4-10%), fatigue (3-8%), and nausea. These are usually mild and go away within an hour. Chest tightness is alarming but rarely dangerous-it’s not a heart attack. Still, if you have heart disease, even mild tightness is a red flag. If side effects are frequent or severe, talk to your doctor about switching to a different triptan or trying a newer medication like a gepant or ditan.



Ruth Witte
December 8, 2025 at 16:16I swear by rizatriptan 🤘 but only if I take it at the FIRST throb. Wait even 10 mins and it’s like trying to put out a forest fire with a water bottle. Also, don’t even get me started on how my hair hurts if I don’t catch it early 😭
Noah Raines
December 10, 2025 at 09:46Triptans are basically magic until they’re not. I’ve had chest tightness so bad I called 911. Turned out it was just the drug. Still, no thanks. I switched to ubrogepant and my life changed. No weird pressure, no dizziness. Just peace. 🙌
Lauren Dare
December 12, 2025 at 08:02Ah yes, the classic 'try a different triptan' advice. Because clearly, if sumatriptan didn't work, the answer is to spend $80 on eletriptan and hope your liver doesn't revolt. Brilliant medical strategy. 🙄
Darcie Streeter-Oxland
December 12, 2025 at 15:06The pharmacological profile of triptans, whilst efficacious in the acute management of migraine, is predicated upon a narrow vasoconstrictive mechanism which may present significant contraindications in patients with cardiovascular comorbidities. One must exercise extreme caution.
Taya Rtichsheva
December 13, 2025 at 20:33so i tried like 4 diff triptans and none worked and then i just started taking ibuprofen with coffee and somehow it works better lmao idk
Michael Robinson
December 14, 2025 at 15:42Pain is the body’s way of saying something’s off. Triptans silence the alarm, but they don’t fix the broken wire. Maybe we should be asking why the wire breaks in the first place.
Kathy Haverly
December 16, 2025 at 03:13Oh wow, another article telling people to 'see your doctor' like that’s the magic solution. Meanwhile, my insurance denies every single gepant, my neurologist won’t return calls, and I’m stuck taking 3 triptans a week just to function. Thanks for the warm words, doc.
Andrea DeWinter
December 17, 2025 at 18:27If you're on an SSRI and your doc prescribes a triptan, ask them if they know about serotonin syndrome. It's rare but real. And if you're using triptans more than 10 days a month, you're probably in MOH territory. Try tracking your attacks. Write down when they start, what you ate, how you slept. It helps more than you think
George Taylor
December 17, 2025 at 19:27Hmm... interesting. The article states that '20% don't respond to any triptan,' yet it doesn't address the fact that most patients are never given a proper trial of multiple triptans-often just one, and then dismissed. Also, the cost barrier is ignored in the 'just try another' section. How convenient.
Lisa Whitesel
December 18, 2025 at 18:00If you're taking triptans more than twice a week you're an addict. Stop blaming the medicine and start blaming yourself.
Larry Lieberman
December 20, 2025 at 17:35Wait so if I have aura should I wait until the pain hits? Like... how do I know when the aura ends and the pain starts? My aura feels like the pain but without the actual headache? 🤔
Michael Robinson
December 22, 2025 at 05:35That’s the thing. Aura isn’t always a warning light. Sometimes it’s the whole damn alarm system going off. The pain starts right when the lights flicker. You learn to feel it. Your body gets good at whispering before it screams.