Cyclosporine Drug Interaction Checker
Enter a medication name to check for interactions with cyclosporine. This tool uses information from the article to provide safety guidance based on CYP3A4 inhibition.
When you take cyclosporine, you’re not just managing your immune system-you’re navigating a minefield of drug interactions. This medication, used after organ transplants and for severe autoimmune conditions like psoriasis or rheumatoid arthritis, doesn’t just sit quietly in your body. It actively interferes with how your liver and gut process other drugs, especially through the CYP3A4 enzyme. And if you don’t understand this, you could end up with toxic levels of another medication-or worse, your transplant could fail.
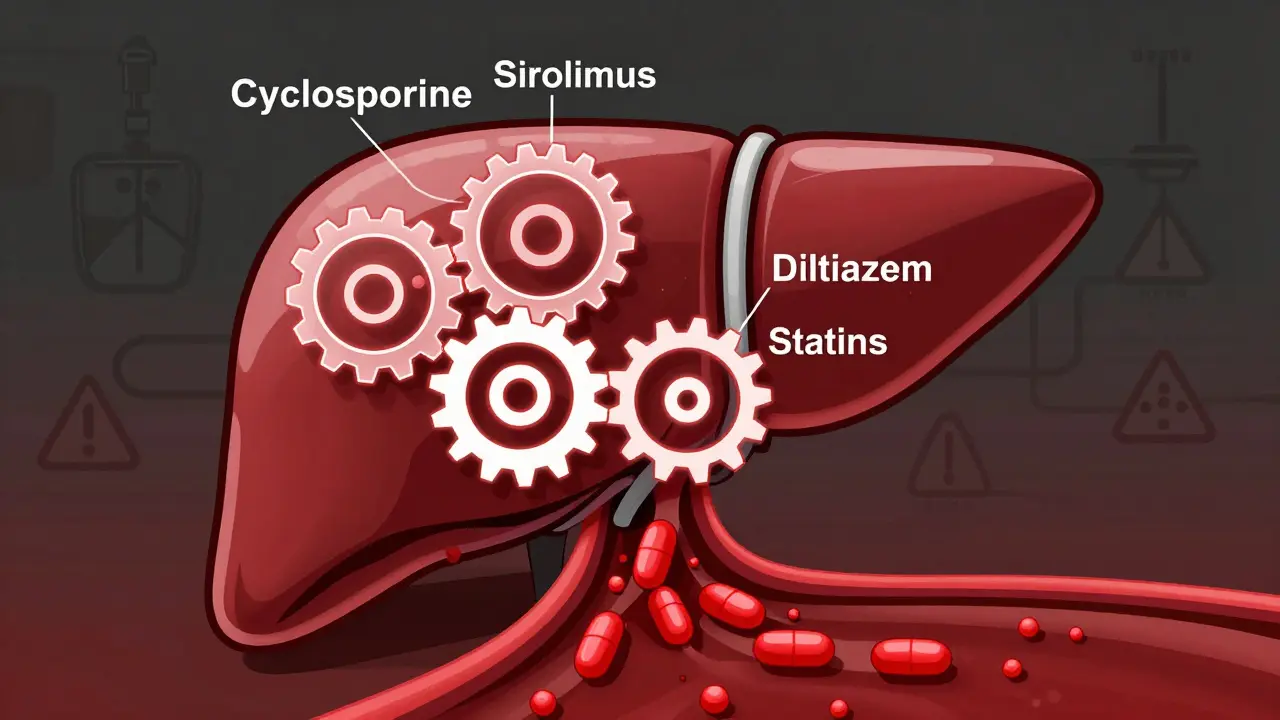
What Cyclosporine Does to Your Liver’s Drug-Metabolizing System
Cyclosporine is both a cyclodepsipeptide and a CYP3A4 inhibitor. That means it doesn’t just get broken down by the CYP3A4 enzyme-it blocks it. CYP3A4 is the most common enzyme in your liver and intestines, responsible for breaking down about 60% of all prescription drugs. When cyclosporine binds to this enzyme, it slows down or stops the metabolism of other drugs that rely on it. The result? Those drugs build up in your bloodstream, sometimes to dangerous levels. This isn’t theoretical. Take sirolimus, another immunosuppressant often used alongside cyclosporine. When taken together, cyclosporine increases sirolimus levels by about 2.2 times. That’s why doctors cut sirolimus doses by 70% when starting it with cyclosporine. Without that adjustment, patients risk severe side effects like mouth sores, lung inflammation, or even kidney damage.Why CYP3A4 Inhibition Isn’t Always Obvious
Many people assume that if a drug interaction is listed, it’s easy to avoid. But cyclosporine’s effect on CYP3A4 is messy. It doesn’t just compete for space on the enzyme like some inhibitors do-it can also cause time-dependent inhibition. That means the longer you take it, the more it disables CYP3A4. This isn’t like flipping a switch; it’s like slowly gluing the enzyme shut. Studies show cyclosporine binds to CYP3A4 in a way that changes its shape permanently, requiring the body to make new enzyme molecules to recover. This is why some interactions don’t show up right away. A patient might start taking diltiazem (a blood pressure pill) and feel fine for a few days-then suddenly their creatinine spikes, their kidneys start struggling, and they’re rushed to the hospital. The cause? Diltiazem is a moderate CYP3A4 inhibitor. Combined with cyclosporine, the two together can cause a 2- to 4-fold increase in cyclosporine blood levels. That’s enough to cause kidney toxicity, high blood pressure, or tremors.What Drugs Are Most Dangerous to Mix With Cyclosporine?
Some medications are so risky with cyclosporine that guidelines say: don’t combine them unless absolutely necessary. Here are the big ones:- Clarithromycin and erythromycin (antibiotics): Strong CYP3A4 inhibitors. One case study showed a renal transplant patient’s cyclosporine levels jumped 300% within 72 hours of starting clarithromycin. Their creatinine rose 60%-a sign of acute kidney injury.
- Fluconazole (antifungal): A moderate inhibitor. Even a single 200mg dose can raise cyclosporine levels by 50%.
- Calcium channel blockers like verapamil and diltiazem: These are commonly prescribed for hypertension or angina. When combined with cyclosporine, they increase the risk of low blood pressure, swelling, and heart rhythm issues.
- Statins like simvastatin and atorvastatin: Used to lower cholesterol. Cyclosporine can cause statin levels to skyrocket, leading to muscle breakdown (rhabdomyolysis), which can permanently damage kidneys.
- Sirolimus, everolimus, and tacrolimus: Other immunosuppressants. Mixing these with cyclosporine is like pouring gasoline on a fire. All three are metabolized by CYP3A4, and cyclosporine turns them into overdoses.
Even over-the-counter drugs like grapefruit juice can be dangerous. Just one glass can inhibit CYP3A4 in the gut for 24 hours, raising cyclosporine levels by up to 50%. Patients are often told to avoid grapefruit entirely while on cyclosporine.

Why Tacrolimus Is Different-And Why It Matters
You might hear doctors say, “We switched you from cyclosporine to tacrolimus because it’s safer.” That’s true-but not for the reason most people think. Tacrolimus doesn’t inhibit CYP3A4. It’s a substrate, meaning it gets broken down by the enzyme, not blocks it. So if you take a CYP3A4 inhibitor like ketoconazole with tacrolimus, your tacrolimus levels rise dangerously. But if you take it with cyclosporine, the opposite happens: cyclosporine doesn’t raise tacrolimus levels the way it raises sirolimus. This distinction is critical. A transplant patient on tacrolimus might be able to safely take a moderate CYP3A4 inhibitor if their levels are monitored. But if they’re on cyclosporine? Even a small dose of an inhibitor can trigger a cascade of side effects. That’s why many centers now prefer tacrolimus as first-line therapy-it’s less likely to cause interactions with other drugs.Genetics Play a Bigger Role Than You Think
Not everyone processes cyclosporine the same way. Your genes matter. The CYP3A4 enzyme has dozens of known variants. Some people have a version called CYP3A4*1B that’s less active. Others have CYP3A5*3, which means they barely produce CYP3A5 at all. Since cyclosporine is metabolized by both CYP3A4 and CYP3A5, people with certain genetic profiles break it down slower-and are more likely to have high blood levels even on standard doses. A 2023 study from Wenzhou Medical University found that patients with specific CYP3A4 variants had up to 40% lower metabolic efficiency. That means their bodies couldn’t clear cyclosporine as quickly. These patients needed lower starting doses to avoid toxicity. Yet, most clinics still use a one-size-fits-all dosing approach. Only a handful of transplant centers in Australia and the U.S. routinely test for these variants before starting therapy.How Doctors Manage These Interactions in Real Life
In a busy transplant clinic, managing cyclosporine interactions isn’t guesswork-it’s a system. Here’s how it works:- Medication review: Every time a patient starts a new drug, the pharmacist checks it against a database of CYP3A4 substrates, inhibitors, and inducers. Even a new antibiotic or antifungal gets flagged.
- Therapeutic drug monitoring: Cyclosporine levels are checked weekly when starting a new drug, then monthly once stable. Trough levels (just before the next dose) are the gold standard. Target range? Usually 100-400 ng/mL, depending on the transplant type and time since surgery.
- Dose adjustments: If a moderate CYP3A4 inhibitor like diltiazem is added, cyclosporine is typically reduced by 25-50%. For strong inhibitors like clarithromycin, the reduction is 50-75%. The goal is to keep levels in the therapeutic range without toxicity.
- Alternative drugs: If possible, doctors switch to drugs that don’t interact. For example, instead of simvastatin, they use pravastatin, which isn’t metabolized by CYP3A4. For fungal infections, they might choose anidulafungin instead of fluconazole.
- Electronic alerts: In hospitals with advanced systems, the EHR automatically flags dangerous combinations. One study showed this cut cyclosporine-related adverse events by 45% across 12 transplant centers.
Still, mistakes happen. A 2021 study of 1,245 kidney transplant patients found that over a third had at least one clinically significant interaction in their first year. Nearly 9% ended up hospitalized because of it.

What You Can Do to Stay Safe
If you’re on cyclosporine, here’s your action plan:- Keep a full list of every medication you take-including vitamins, supplements, and herbal products. St. John’s wort, for example, is a strong CYP3A4 inducer and can cause transplant rejection.
- Never start a new drug without talking to your transplant team. Even OTC painkillers like ibuprofen can stress your kidneys when combined with cyclosporine.
- Avoid grapefruit, pomelo, and Seville oranges. They’re not just fruit-they’re chemical disruptors.
- Know your cyclosporine levels. Ask your doctor to show you your last trough result. If you don’t know what it is, you’re flying blind.
- Ask if you can be tested for CYP3A4 or CYP3A5 genetic variants. It’s not routine everywhere, but it’s becoming more common-and it could save your life.
The Bigger Picture: Why Cyclosporine Still Matters
You might think cyclosporine is outdated. After all, tacrolimus is more effective and has fewer interactions. But cyclosporine is still used in about 30% of adult transplants and nearly half of pediatric cases. It’s cheaper. It’s better tolerated in some autoimmune diseases. And in places with limited access to newer drugs, it’s often the only option. The global market for cyclosporine was worth $1.87 billion in 2022 and is expected to grow 3.2% per year through 2030. That’s not because it’s perfect-it’s because when used right, it saves lives. But “used right” means understanding its power to alter how every other drug behaves in your body.Future Changes: Personalized Dosing Is Coming
Researchers are now building algorithms that predict cyclosporine levels based on your genetics, age, weight, kidney function, and current medications. Early versions are 85-90% accurate. One prototype device being tested in Melbourne can measure cyclosporine levels from a single drop of blood in under 10 minutes-with results matching lab tests at r=0.95. Imagine walking into your clinic, getting a finger prick, and knowing your dose needs to change before you even sit down. The FDA and European transplant societies are pushing for these tools to become standard. Because in a world of complex drug interactions, guesswork is no longer acceptable.Can I take ibuprofen with cyclosporine?
It’s not recommended. Ibuprofen and other NSAIDs can reduce kidney blood flow, and cyclosporine already stresses the kidneys. Together, they raise the risk of acute kidney injury. If you need pain relief, acetaminophen (paracetamol) is safer-but always check with your doctor first.
Does grapefruit juice really affect cyclosporine?
Yes, and it’s dangerous. Grapefruit contains compounds that block CYP3A4 in the gut, causing cyclosporine levels to spike by up to 50%. Even a single glass can have effects that last 24 hours. Avoid grapefruit, pomelo, and Seville oranges entirely while on cyclosporine.
Why do I need blood tests if I feel fine?
Cyclosporine has a narrow therapeutic window. You can have toxic levels without feeling sick. Symptoms like tremors, high blood pressure, or kidney changes often appear only after damage is already happening. Blood tests catch these changes early-before you feel anything.
Is cyclosporine being replaced by other drugs?
Tacrolimus is now preferred for most transplants because it’s more effective and has fewer drug interactions. But cyclosporine is still used in children, patients with certain autoimmune diseases, and in regions where newer drugs are too expensive. It’s not obsolete-it just requires more careful management.
Can I take herbal supplements with cyclosporine?
No. Many herbs like St. John’s wort, echinacea, and garlic can interfere with CYP3A4. St. John’s wort is a strong inducer-it can drop cyclosporine levels by 50-80%, leading to organ rejection. Always tell your doctor about every supplement you take.
What should I do if I miss a dose of cyclosporine?
If you miss a dose, take it as soon as you remember-unless it’s close to your next scheduled dose. Never double up. Missing doses can cause rejection, but taking too much can cause toxicity. Always follow your transplant team’s specific instructions.
If you’re on cyclosporine, your safety depends on awareness-not luck. Know your drugs. Know your levels. And never assume a new medication is safe just because it’s over-the-counter or prescribed by a different doctor.



Roshan Gudhe
February 5, 2026 at 02:18Cyclosporine is one of those drugs that makes you realize medicine isn't just about pills-it's about systems. The way it glues CYP3A4 shut like industrial glue? That's not pharmacology, that's biochemistry horror fiction. And yet, people still take grapefruit juice like it's a health trend. We're not just patients-we're walking pharmacokinetic experiments.
Janice Williams
February 5, 2026 at 03:00It's fascinating how this entire field is built on the assumption that patients are capable of understanding complex pharmacology. Meanwhile, the average person can't even spell 'CYP3A4'-let alone know what it does. This isn't medicine-it's a high-stakes game of Russian roulette with a prescription pad.
Joy Johnston
February 5, 2026 at 05:12As a pharmacist, I see this every day. A patient comes in with a new script for diltiazem and no idea they're on cyclosporine. We catch it before the creatinine spikes, but it's terrifying how often we don't. The system isn't broken-it's just under-resourced. We need better EHR alerts, better education, and better communication between specialists. It's not rocket science, but it feels like it sometimes.
Kunal Kaushik
February 7, 2026 at 04:53Man, I had a cousin on cyclosporine after his kidney transplant. He swore off grapefruit like it was poison-and he was right. But he also started taking turmeric supplements because 'it's natural.' We had to pull him off it. Turns out, natural doesn't mean safe. Just because it's from a plant doesn't mean it won't mess with your meds.
Caleb Sutton
February 8, 2026 at 23:56They don't want you to know this, but cyclosporine is a control mechanism. Big Pharma pushes it because it forces lifelong monitoring, blood tests, and doctor visits. It's not about health-it's about profit. The 'genetic testing' they mention? That's a gimmick to sell more tests. They want you dependent. Always watching. Always afraid.
Jamillah Rodriguez
February 9, 2026 at 10:09Okay but why is everyone so obsessed with CYP3A4? Like, can't we just… not take drugs? 🤔 I mean, if it's this dangerous, maybe we should just stop mixing things and live in a cave. Also, grapefruit juice is gross anyway. 🍊❌
Susheel Sharma
February 10, 2026 at 08:27The real tragedy here isn't the drug interactions-it's the institutional laziness. A 2021 study found 33% of transplant patients had dangerous interactions? That’s not negligence-that’s systemic malpractice. And yet, most clinics still use dosing tables from the 1990s. We have AI, genomics, real-time monitoring-and we’re still winging it like it’s 1987. Shameful.
Rachel Kipps
February 10, 2026 at 23:53i just read this and my head is spinning. i had no idea grapefruit could do that. i thought it was just bad for your teeth. and the part about tacrolimus being different? that actually made sense. i’m gonna print this out and show my doctor. thanks for writing this. really.
Katherine Urbahn
February 12, 2026 at 12:14Let me be perfectly clear: if you are taking cyclosporine, and you are consuming ANY substance-prescription, over-the-counter, herbal, or dietary-that has even a remote possibility of interacting with CYP3A4, you are not just being careless-you are endangering your life, your family, and your healthcare system. There is no excuse. None. Period.
Shelby Price
February 12, 2026 at 16:42Wait-so if tacrolimus doesn’t block CYP3A4, why do they still test levels so often? Isn’t it just a substrate? So if someone takes a CYP3A4 inhibitor with tacrolimus, it’s the inhibitor’s fault, not tacrolimus’s? That’s wild. I always thought they were the same. Thanks for clarifying. 🤯
Jesse Naidoo
February 14, 2026 at 06:49My brother died because of this. They switched him to tacrolimus after his transplant, but then gave him fluconazole for a yeast infection. No one told him. No one checked his levels. He was fine one day, gone the next. This isn’t just info-it’s a warning. Don’t let this happen to you.
Sherman Lee
February 15, 2026 at 11:45They say genetic testing is coming-but they’ve been saying that for 15 years. Meanwhile, your doctor still guesses your dose based on your weight and a hunch. This whole system is a house of cards. And the real question is: who’s paying for all these blood tests? Hint: not you. Not yet.
Lorena Druetta
February 16, 2026 at 00:27Reading this made me so grateful for my transplant team. They sit with me for an hour every visit, explain every new pill, and never make me feel stupid for asking. If you're on cyclosporine-find a team like this. It’s not just medicine. It’s your lifeline.
Zachary French
February 16, 2026 at 23:23So let me get this straight: cyclosporine is basically a drug that turns your liver into a drug-sucking black hole, and we're still using it because it's CHEAPER? That's not a medical decision-that's a corporate crime. And don't even get me started on how they're gonna 'personalize dosing' next year. Yeah, right. Like the FDA gives a damn until someone dies. This whole system is rigged.