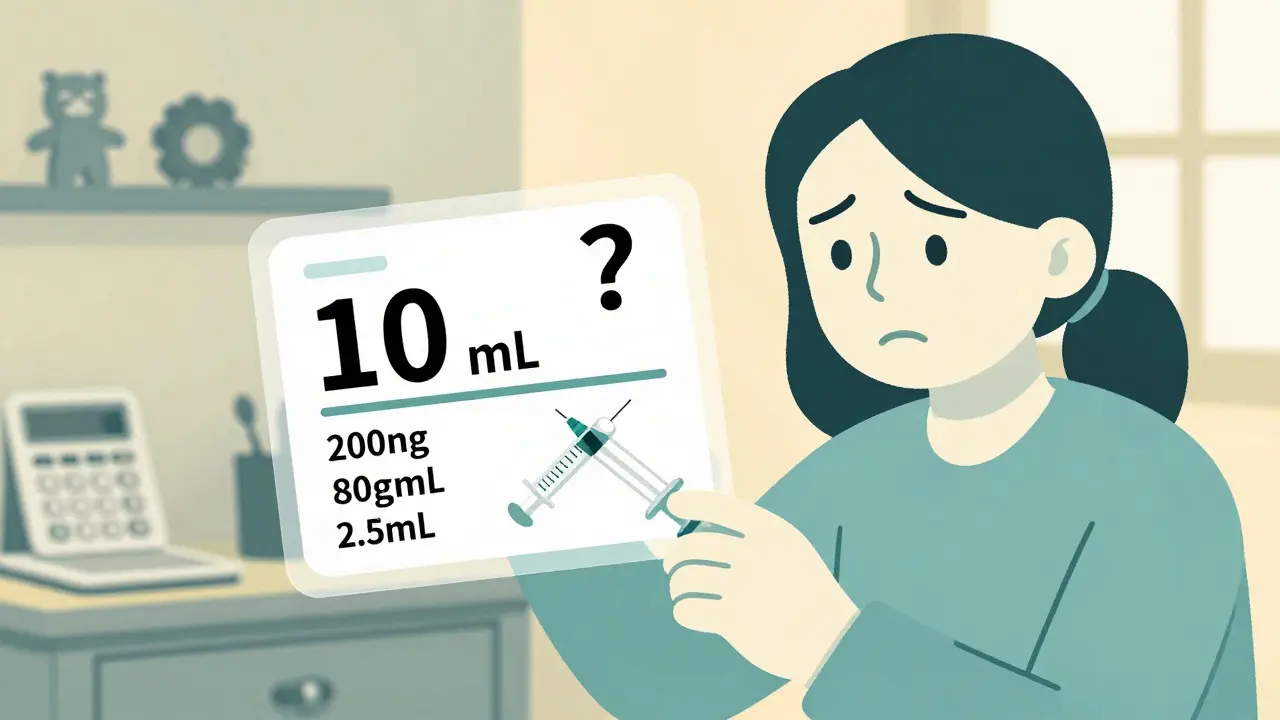
When your child gets a new prescription, the label might say 10 mL - but what does that actually mean? Is it 10 milliliters of medicine, or 10 milligrams of active drug? If you’re not sure, you’re not alone. Thousands of parents face this confusion every day, and the stakes couldn’t be higher. A wrong dose can mean a trip to the ER - or worse. Confirming pediatric dosing isn’t just a step in the process; it’s the most important safety check you’ll ever make for your child’s health.
Why Pediatric Dosing Is Different
Children aren’t small adults. Their bodies process medicine differently. A dose that’s safe for a 150-pound teen could be deadly for a 20-pound toddler. That’s why pediatric dosing relies on weight, not age. The standard method is milligrams per kilogram (mg/kg), meaning the amount of medicine is calculated based on how much the child weighs - not how old they are. The American Society of Health-System Pharmacists (ASHP) and the American Academy of Pediatrics (AAP) both require this approach for all children under 12. Even for older kids, weight-based dosing is the gold standard.
According to the Institute for Safe Medication Practices (ISMP), pediatric patients suffer medication errors at 3 times the rate of adults. And over half of those errors - 56% - are dosing mistakes. Many come from simple mix-ups: confusing milliliters (mL) with milligrams (mg), using the wrong concentration, or misreading the weight on the label.
What to Look for on the Prescription Label
Every pediatric prescription label should include three non-negotiable pieces of information:
- The child’s actual weight in kilograms (kg)
- The exact dose in milligrams (mg) per administration
- The concentration of the liquid (e.g., 80 mg/mL or 160 mg/5 mL)
If any of these are missing, stop. Don’t fill the prescription. Call the pharmacy or prescriber. A label that says "Give 10 mL" without stating the mg amount is unsafe. The FDA’s 2021 Drug Safety Communication requires all liquid pediatric medications to show both metric (mg) and non-metric (mL) measurements - but many older prescriptions still slip through.
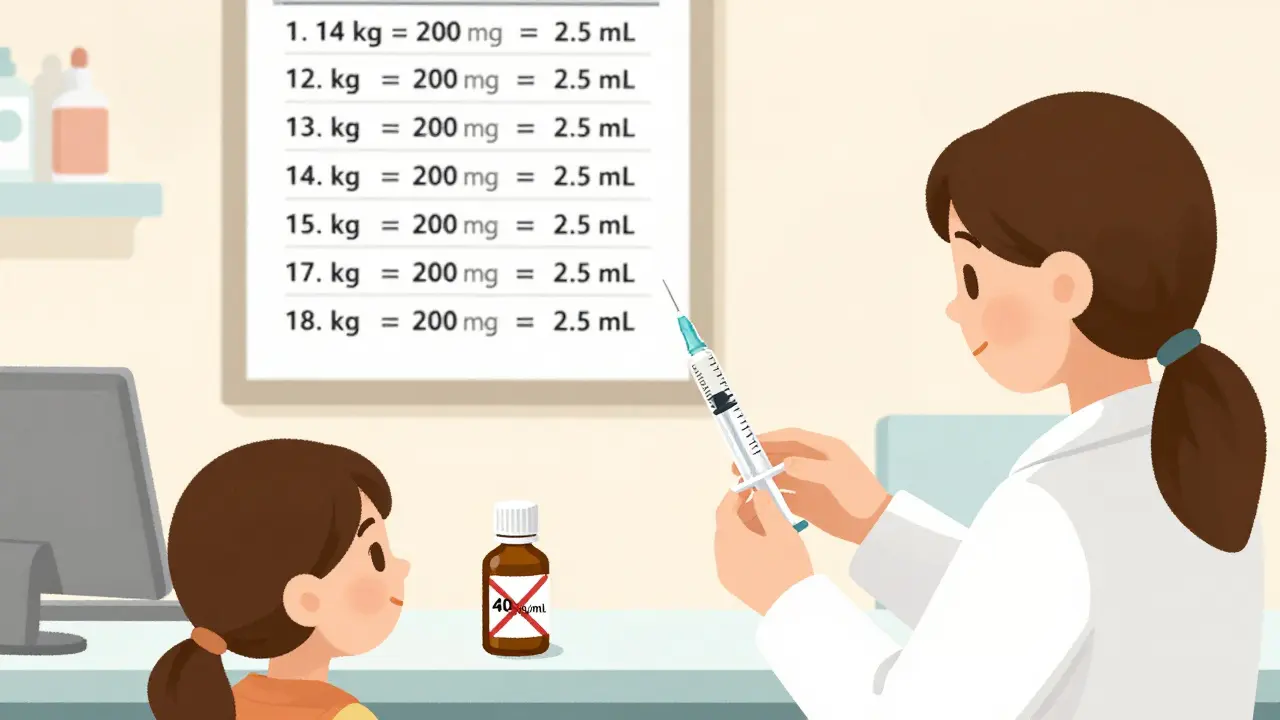
Here’s what a properly labeled pediatric prescription should look like:
- Child’s weight: 14 kg
- Dose: 200 mg
- Concentration: 80 mg/mL
- Frequency: Twice daily
- Volume to give: 2.5 mL
Notice how the volume (2.5 mL) is clearly tied to the dose (200 mg) and the concentration (80 mg/mL). That’s the connection you need to verify.
How to Check the Dose Yourself
You don’t need to be a doctor to catch a dosing error. Here’s how to do it in four simple steps:
- Convert pounds to kilograms - If the label shows weight in pounds, divide by 2.2. For example, a 33-pound child is 33 ÷ 2.2 = 15 kg. Never guess. Use a calculator.
- Find the prescribed dose in mg - Look for "mg" or "milligrams." If it only says "mL," ask for clarification. A common error is when a child gets 10 mL of a 160 mg/5 mL solution - that’s 320 mg, not 10 mg.
- Calculate the dose based on weight - Multiply the child’s weight (kg) by the recommended dose per kg. For amoxicillin, it’s often 40-50 mg/kg/day. So a 15 kg child would get 600-750 mg per day, split into two doses (300-375 mg each).
- Match the volume to the concentration - If the dose is 200 mg and the concentration is 80 mg/mL, divide 200 by 80 = 2.5 mL. Use the syringe provided. Never use a kitchen spoon.
For example: A 4-year-old weighing 16 kg is prescribed amoxicillin at 45 mg/kg/day. Total daily dose = 16 × 45 = 720 mg. Divided into two doses = 360 mg per dose. If the concentration is 80 mg/mL, each dose = 360 ÷ 80 = 4.5 mL. If the label says "Give 5 mL," you’re giving 400 mg - close enough. But if it says "10 mL," that’s 800 mg - nearly double the dose. That’s a red flag.
Common Mistakes That Put Kids at Risk
These errors happen more often than you think:
- Confusing concentration - Amoxicillin comes in 40 mg/mL, 80 mg/mL, and 125 mg/5 mL. Mixing them up can lead to 2x-3x overdoses. Always check the bottle label.
- Using wrong units - "Give 10 mL" without mg is dangerous. A 2022 study found 43.5% of preventable adverse events came from mg/mL confusion.
- Incorrect weight conversion - 22 lb is not 10 kg - it’s 10 kg. A 2.2 lb = 1 kg ratio is exact. Many parents and even some nurses use 2 lb = 1 kg, which leads to 10% under-dosing.
- Rounding errors - Some EHR systems round doses. Cerner rounds doses under 10 mg to the nearest 0.1 mg. EPIC rounds higher doses to whole numbers. Always compare the ordered dose to the actual dose dispensed.
One mother on Reddit shared a near-miss: Her 4-year-old’s prescription said "10 mL" of amoxicillin. She thought it was too little. She checked the concentration - 80 mg/mL - and realized the dose should’ve been 200 mg (2.5 mL), not 10 mL (800 mg). She called the pharmacy. The dose was corrected. That’s how you save a life.
What Parents Should Ask
Don’t be shy. Ask these three questions every time:
- "What is the exact dose in milligrams?" - Not mL. Not teaspoons. Milligrams.
- "Is this dose appropriate for my child’s current weight?" - If they say "it’s standard," ask for the calculation. A 15 kg child shouldn’t get the same dose as a 25 kg child.
- "Can you show me how to measure this with the syringe?" - Pharmacists should demonstrate. If they hand you a syringe without explaining, walk out.
These aren’t "annoying" questions. They’re lifesavers. The American College of Clinical Pharmacy says 94.8% of calculation errors during prescribing can be caught with better communication. You’re not second-guessing the doctor - you’re helping them do their job right.
Technology Is Helping - But You Still Need to Double-Check
Hospitals are using smart systems to cut errors. EPIC and Cerner now flag mismatched doses. DoseSpot’s AI tool checks 15,000+ dosing guidelines and catches 99.2% of mistakes. The SMART on FHIR standard lets EHRs auto-verify doses as doctors type.
But here’s the truth: technology doesn’t replace human verification. A 2023 study in the Journal of Pediatric Pharmacology found that 71% of system alerts were ignored because staff assumed the computer was right. Parents are the last line of defense. If your child’s label doesn’t clearly show mg/kg, or if the dose seems off, speak up.
What to Do If Something Feels Wrong
Trust your gut. If the dose looks too small - it might be right. If it looks too big - it might be wrong. A nurse with 12 years of ICU experience once said: "The most dangerous thing is when parents think a dose is too small for their child and don’t question it." A 5 mL dose might seem like a lot - but for a 30 kg child on a high-dose antibiotic, it could be exactly right.
Here’s what to do:
- Call the pharmacy. Ask to speak to the pharmacist - not the technician.
- Ask them to walk you through the calculation.
- If they can’t explain it clearly, ask for a written dose sheet.
- If the issue isn’t resolved, call the prescribing provider.
Never give a dose you’re unsure about. Even one extra milligram can be dangerous for a baby. Better to wait an hour than risk a hospital stay.
Final Checklist Before Giving the Dose
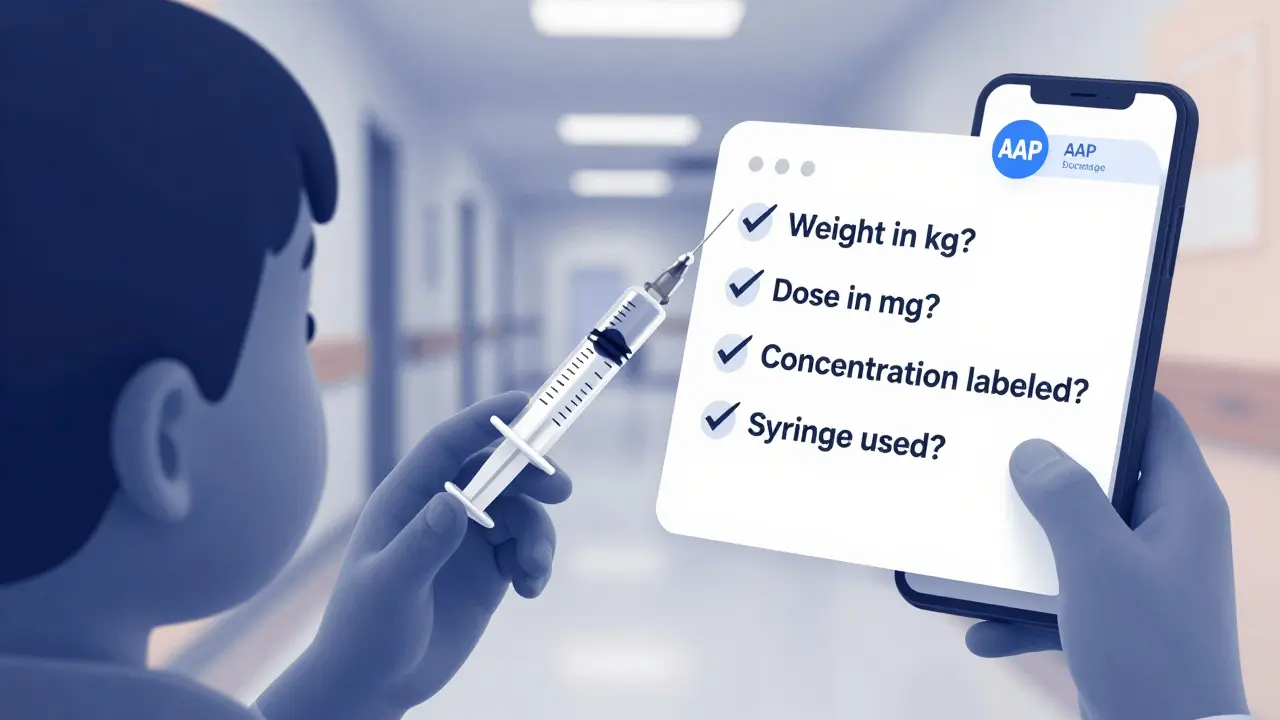
Before you give your child any medication, run through this quick checklist:
- ✅ Child’s weight is listed in kg (not lbs)
- ✅ Dose is written in mg (not mL)
- ✅ Concentration is clearly labeled (e.g., 80 mg/mL)
- ✅ Volume to give matches the mg dose and concentration
- ✅ You used the provided syringe - not a spoon or cup
- ✅ You’ve confirmed the dose with at least one other adult or reference
Keep a printed copy of the manufacturer’s dosing chart in your wallet. Many pharmacies give them out. Or download the AAP’s pediatric dosing app. It’s free, updated yearly, and works offline.
What if the prescription label doesn’t list my child’s weight in kilograms?
Stop. Do not fill the prescription. Call the prescribing doctor or pharmacy immediately. A valid pediatric prescription must include the child’s weight in kilograms. If it doesn’t, it’s incomplete and unsafe. The American Academy of Pediatrics’ 2024 policy requires this information on all pediatric prescriptions.
Can I use a kitchen teaspoon to measure liquid medicine?
Never. Kitchen spoons vary in size - a teaspoon can hold anywhere from 2.5 mL to 7 mL. Always use the syringe or dosing cup provided with the medication. These are calibrated for accuracy. A 2021 CDC report found that using non-medical measuring tools caused 37% of dosing errors in children under 2.
Why do some liquid medicines have two concentrations?
Manufacturers make different concentrations to make dosing easier for different age groups. For example, amoxicillin comes as 40 mg/mL for infants and 80 mg/mL for older children. Using the wrong one can cause a 2x overdose. Always check the concentration on the bottle and match it to the prescription. Never assume they’re the same.
Is it safe to give my child half of an adult dose?
No. Adult doses are not scaled down by half. Children need doses based on weight, not age or size. A 20-pound child may need less than 1/4 of an adult dose. A 70-pound teen might need nearly the full adult dose. Always use a weight-based calculation. Clark’s rule (using 150 lbs as a reference) is outdated and inaccurate.
How do I know if the pharmacy gave me the right concentration?
Check the bottle label. The concentration must match what’s on the prescription. If the script says 80 mg/mL but the bottle says 40 mg/mL, ask the pharmacist to confirm. They may have substituted a different formulation. Always verify the mg/mL number before leaving the pharmacy.

Marie Fontaine
February 11, 2026 at 09:06This is so important! I once gave my kid the wrong dose because I thought '10 mL' meant 10 mg. Thank you for spelling this out so clearly. I'm printing this out and taping it to the fridge. 🙌
Brandon Osborne
February 12, 2026 at 11:58I can't believe pharmacists still hand out labels that just say 'give 10 mL' like it's a goddamn riddle. My daughter almost died because some tech didn't bother to write the mg. I called the FDA. I called the state board. I called the doctor's office at 2 a.m. I'm not done fighting. If you're not asking for the mg, you're gambling with your kid's life. Period.
Susan Kwan
February 12, 2026 at 20:05Oh wow. Another post telling parents they need to be pharmacists now. Let me guess-next you'll be asking us to interpret EHR alerts and calculate Clark's Rule on the fly. Meanwhile, the system still doesn't auto-calculate weight-based doses in 80% of pediatric clinics. You're blaming parents for a broken system. How about we fix the damn labels first?
Chelsea Cook
February 14, 2026 at 05:50Y'all are killing it with this thread. I'm a nurse and I've seen so many parents panic because they're not sure if they're giving the right amount. The fact that you're even asking these questions means you're already doing better than 90% of caregivers. Keep asking. Keep double-checking. You're not being annoying-you're being heroic. 💪❤️
Jacob den Hollander
February 14, 2026 at 07:05i just want to say thank you for this post. i'm a dad of two, and honestly i never knew about the kg vs lb thing until now. i always thought 20 lbs = 10 kg but now i know it's 9.07. i'm gonna write this down on my phone. also, i'm gonna ask the pharmacist to show me how to use the syringe next time. i feel so much better already. thanks again. 🙏
Chima Ifeanyi
February 14, 2026 at 09:33The entire premise is a neoliberal fallacy. The burden of pharmaceutical literacy is being externalized onto marginalized caregivers while systemic failures persist. The 56% error rate you cite is a direct consequence of underfunded public health infrastructure, not parental negligence. You're pathologizing caretaking behavior while ignoring the structural violence embedded in pharmaceutical distribution networks. Also, amoxicillin concentration isn't standardized globally-your US-centric model is ethnocentric.
THANGAVEL PARASAKTHI
February 15, 2026 at 23:42this is great but i think u missed one thing: in india we get liquid meds in dropper bottles and sometimes the dropper is not calibrated. i had to use a syringe from my son's last prescription because the new one had a weird dropper. also, concentration on bottle was faded. i had to call the pharmacy twice. pls add a note about checking the dropper too.
Chelsea Deflyss
February 16, 2026 at 09:20I'm sorry but if you can't figure out 10 mL vs 10 mg, maybe you shouldn't be giving your kid medicine. I've seen too many parents who treat prescriptions like they're guessing at a game show. You don't get a prize if you guess right-you get an ER visit. Stop being lazy. Read the label. Use the syringe. Or don't give the medicine at all.
Tricia O'Sullivan
February 17, 2026 at 02:58I must express my profound appreciation for the clarity and precision of this exposition. The systematic delineation of weight-based dosing parameters, coupled with the explicit enumeration of concentration metrics, constitutes a model of clinical communication. I shall retain this document in my personal medical archive for future reference. Thank you for upholding the highest standards of patient safety.
Scott Conner
February 18, 2026 at 13:57i was just about to fill my daughter's script when i saw this. thanks for the 4 step thing. i did the math and realized the label said 10ml but it shouldve been 3.5ml. i called the pharmacy and they were like 'oh yeah we messed up' and fixed it. i feel like a superhero right now. also i used the syringe. no spoon. ever again.
Lyle Whyatt
February 20, 2026 at 06:25Look, I get it. You're trying to help. But let’s be real here. The system is broken. I work in a hospital pharmacy. We have 17 different concentrations of amoxicillin on the shelf. The EHR auto-populates based on the prescriber’s default setting, which is often outdated. The nurse who dispenses it? She’s got 3 kids, 2 jobs, and 12 patients on her cart. She doesn’t have time to explain concentration ratios. So you, the parent, get left holding the bag. I’ve seen parents cry because they thought they were overdosing. I’ve seen them give half the dose because they were terrified. We need standardized labeling. We need mandatory pharmacist counseling. We need a national pediatric dosing database. This checklist? It’s a bandaid. And I’m not mad at you for using it. I’m mad at the system that forces you to.
Ken Cooper
February 21, 2026 at 12:04i just wanna say thank you for this. i read it twice. i printed it. i showed my wife. we have a 3 year old and we were so confused last time. the pharmacy gave us a bottle that said 80 mg/ml but the script said 40 mg/ml. we didn't know which one to trust. we called the doctor and he said 'oh that's the new formulation' but didn't change the script. we almost gave the wrong dose. i'm so glad i found this. i'm gonna put it on the fridge next to the crayons. ps: i spelled 'milligram' wrong 3 times. sorry.
MANI V
February 23, 2026 at 03:15This is the same garbage I've been seeing since 2018. 'Just ask for the mg!' Like that's going to happen when the pharmacist is on the phone with the insurance company and the doctor's office is closed. You're not protecting children-you're just making parents feel guilty. The real problem? Drug companies making 3 different concentrations. The real problem? Pharmacies not updating labels. The real problem? No one holding them accountable. This checklist? It's a distraction. A performative safety ritual for people who think they're doing enough.