When pain becomes constant, it’s easy to spiral. Your mind starts racing: What if this never gets better? What if I can’t work again? This is going to destroy my life. These aren’t just passing thoughts-they’re patterns. And they’re making the pain worse. This is pain catastrophizing, and it’s not just in your head. It’s a real, measurable psychological response that amplifies physical suffering. The good news? You don’t have to stay stuck in this cycle. Cognitive Behavioral Therapy (CBT) gives you practical, science-backed tools to break it.
What Exactly Is Pain Catastrophizing?
Pain catastrophizing isn’t being dramatic. It’s a specific pattern of thinking that kicks in when you’re in pain-or even when you expect it. Researchers define it as an exaggerated negative mindset toward pain, made up of three parts: rumination (can’t stop thinking about it), magnification (believing it’s worse than it is), and helplessness (feeling like you can’t do anything about it). The Pain Catastrophizing Scale (PCS), developed in the 1990s, measures this. If you score 30 or higher out of 52, you’re experiencing clinically significant catastrophizing. That’s not rare. Studies show up to 40% of people with chronic pain score in this range. And it’s not just about feeling down-it’s linked to higher pain intensity, longer recovery times, and even increased risk of depression and suicidal thoughts. Here’s the key insight: catastrophizing doesn’t just happen because you’re in pain. It actually makes the pain feel worse. Brain scans show that when you’re catastrophizing, areas involved in emotion and pain processing light up more. Your thoughts are literally changing how your body experiences pain.How CBT Breaks the Cycle
CBT doesn’t tell you to “think positive.” It doesn’t ignore your pain. Instead, it helps you separate what’s actually happening in your body from the story your mind is telling you about it. Think of it like this: You feel a sharp ache in your lower back. Your brain immediately jumps to: “This is a herniated disc. I’m going to end up in a wheelchair. I’ll never play with my kids again.” That’s catastrophizing. CBT teaches you to pause and ask: “Is that fact, or is that fear?” The process works in three stages:- Awareness - You start tracking your thoughts when pain flares. Not just “I hurt,” but “I’m thinking I’ll never get better, and I’m scared to move.”
- Challenge - You look at those thoughts like a detective. What’s the evidence? Has this happened before? What’s the most realistic outcome?
- Replace - You swap the worst-case story for a more balanced one: “This pain is intense, but it’s not new. I’ve managed it before. I can take it slow.”
Three CBT Tools You Can Start Using Today
You don’t need a therapist to begin. These tools are used in VA clinics, pain centers, and digital apps like Curable and PainScale-and they work.1. Thought Records
Grab a notebook or use your phone. When pain spikes, write down:- What happened? (e.g., “Stood up from chair, felt sharp pain in hip.”)
- What did I think? (e.g., “This means my arthritis is destroying my joint. I’ll need surgery.”)
- How did I feel? (e.g., “Panicked, tense, froze in place.”)
- What did I do? (e.g., “Sat down and didn’t move for an hour.”)
- What’s a more realistic thought? (e.g., “I’ve had this pain before. It’s flare-up, not damage. Moving slowly will help.”)
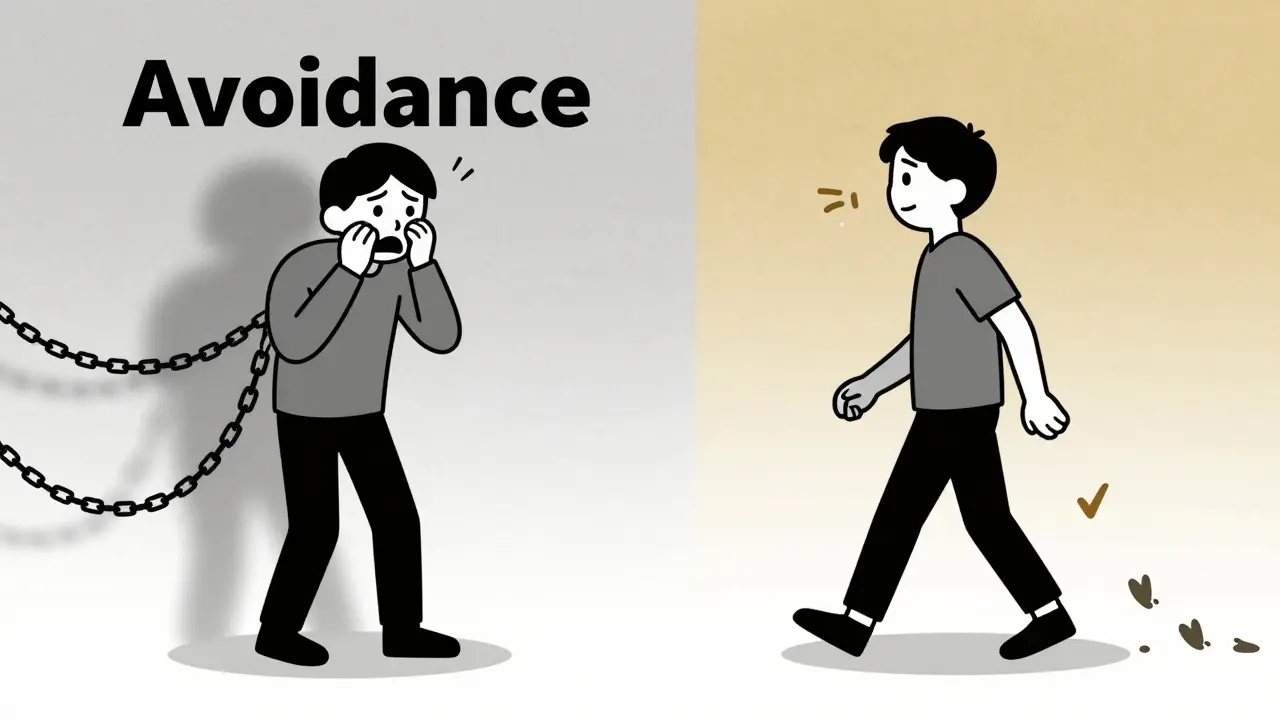
2. Behavioral Activation
Catastrophizing makes you avoid movement. But avoidance = more pain over time. CBT flips this by gently pushing you back into activity-not all at once, but in small, manageable steps. Start with a simple goal: “Walk for 5 minutes, twice today.” Not “I’ll walk until I feel better.” That’s setting yourself up to fail. Track your activity and your pain level on a scale of 1-10. You’ll likely notice: “I thought walking would make it worse, but after 5 minutes, it actually felt a little better.” That’s your brain learning that movement isn’t a threat. A 2024 VA study found that combining CBT with light movement reduced catastrophizing scores by 32% in 12 weeks. The movement wasn’t intense-it was consistent.3. Grounding for Overwhelm
When your pain hits an 8 or 9, your brain can’t handle complex thinking. That’s when you need a simple anchor. Try the 5-4-3-2-1 technique:- Name 5 things you can see
- Name 4 things you can touch
- Name 3 things you can hear
- Name 2 things you can smell
- Name 1 thing you can taste
What Doesn’t Work (And Why)
Some people try to “just relax” or “stay positive.” That’s not CBT. It’s avoidance with a smile. Others think CBT means “your pain isn’t real.” It’s the opposite. CBT says your pain is real-but your thoughts about it are making it worse. You’re not being weak. You’re stuck in a loop that’s hard to break without tools. Also, CBT isn’t magic. It takes time. Most people start seeing changes after 3-4 weeks. Full results often take 8-12 weeks. If you quit because you didn’t feel better right away, you’ll miss the payoff. And yes-some days, when your pain is crushing, you won’t have the mental energy to do a thought record. That’s normal. On those days, just do one thing: breathe. Move a little. Don’t punish yourself. Progress isn’t linear.Who Benefits Most?
CBT works best for people who:- Have chronic pain (not just acute injury)
- Feel stuck in a cycle of fear and avoidance
- Are willing to track their thoughts and actions
- Have some mental bandwidth to engage, even if limited

Getting Started
You don’t need to wait for a referral. Start today.- Download a free thought record template online (VA or PainScience.com have them).
- Try the 5-4-3-2-1 grounding technique the next time pain spikes.
- Walk for 5 minutes-even if you think it’ll hurt. Write down what happened.
Real Stories
On Reddit’s r/ChronicPain, users report that after 8-12 weeks of CBT, 78% saw a drop in distress. One user wrote: “I used to cry before I even got out of bed. Now I say, ‘Okay, pain’s here. I’m not letting it steal my whole day.’” Another said: “I thought CBT was just talking. Turns out, it’s about rewiring how I react. My pain didn’t vanish. But my fear did. And that changed everything.” The science backs this up. CBT has the largest effect size for reducing pain catastrophizing compared to any other therapy. It’s not just popular-it’s proven.What’s Next?
By 2025, 75% of pain clinics will screen for catastrophizing. Digital CBT apps are exploding. Researchers are even testing smartphone alerts that pop up when you’re likely catastrophizing-offering a quick grounding exercise right then and there. But the core won’t change. Pain catastrophizing is a learned pattern. And like any learned pattern, it can be unlearned. You don’t need to fix your pain. You just need to stop letting your thoughts make it worse. Start small. Be consistent. Track your progress. And remember-you’re not broken. You’re just caught in a cycle that CBT was designed to break.Is pain catastrophizing the same as being depressed?
No. While they often overlap, pain catastrophizing is a specific thinking pattern focused on pain-like believing it will never end or that you can’t handle it. Depression is a broader mood disorder. Someone can catastrophize without being clinically depressed, and vice versa. But catastrophizing can lead to depression over time, which is why treating it early matters.
Can CBT make my pain worse at first?
It’s possible, but rare. Some people feel more emotional discomfort at first because they’re finally facing thoughts they’ve been avoiding. This doesn’t mean the pain is getting worse-it means you’re becoming aware of how your mind is amplifying it. That discomfort usually fades within a few weeks as you gain tools to manage it.
Do I need a therapist to do CBT for pain catastrophizing?
You don’t need one, but it helps. Many people successfully use self-guided apps, books, or worksheets. But if you’re struggling to identify thoughts, feel overwhelmed, or have other mental health concerns, working with a trained CBT therapist increases your chances of success. Look for someone with experience in chronic pain.
How long until I see results from CBT?
Most people notice small shifts in 3-4 weeks-like catching a catastrophic thought before it spirals. Meaningful changes in pain distress and function usually take 8-12 weeks. It’s not a quick fix, but the results last longer than medication.
What if I can’t focus during high-pain episodes?
That’s normal. On high-pain days, skip the thought records. Use grounding techniques instead-like 5-4-3-2-1 or slow breathing. The goal isn’t to fix everything at once. It’s to build skills over time so you can use them when you’re able. Even small efforts count.



Darren McGuff
January 9, 2026 at 10:37Let me tell you something real: I’ve been living with chronic back pain for 12 years. I tried everything-steroids, acupuncture, even a damn spinal stimulator. Nothing stuck until I started doing thought records. Not because it ‘fixed’ my spine, but because it stopped my brain from turning every twinge into a funeral. I used to cancel plans just to lie there and dread the next hour. Now? I walk my dog for 7 minutes. That’s it. And I don’t feel guilty about it. That’s the real win.
CBT didn’t make me ‘positive.’ It made me honest. And honesty? That’s the only thing that actually reduces pain.
Also, if you’re reading this and thinking ‘I’m not that bad,’ you’re lying to yourself. We all do it. The trick is catching it before it catches you.
Jacob Paterson
January 11, 2026 at 08:13Of course this works. Because nothing says ‘I’m not broken’ like being told your pain is just bad thinking.
Next they’ll tell me my broken leg is just a negative thought pattern. Real helpful, genius.
Micheal Murdoch
January 13, 2026 at 02:34Jacob, I get it. You’re angry. And you’re not wrong to be. Pain is real. It’s brutal. It steals your identity, your independence, your sleep.
But CBT isn’t denying that. It’s saying: ‘Yes, this hurts. And yes, your mind is screaming that it will never end. But what if that scream is lying?’
I lost my job because I couldn’t sit through a meeting. I thought I was broken. Turns out, I was just trapped in a loop of ‘this is it, I’m done.’ CBT didn’t fix my spine. It fixed my relationship with the pain. And that’s everything.
You don’t have to believe it today. But don’t dismiss it because it doesn’t fit your idea of ‘real healing.’ Sometimes the deepest wounds aren’t in the body-they’re in the stories we tell ourselves about it.
Heather Wilson
January 14, 2026 at 13:11Let’s be honest-this whole CBT-for-pain thing is just another form of victim-blaming disguised as science. You’re telling people with degenerative disc disease or fibromyalgia that their suffering is ‘in their head’? That’s not therapy, that’s gaslighting.
I’ve seen too many patients get told to ‘just think differently’ while their insurance refuses to cover surgery or nerve blocks. CBT is the cheap alternative. The lazy solution. The ‘we don’t have the resources so just cope’ excuse.
And don’t give me that ‘it’s not denying pain’ crap. The language is designed to make people feel guilty for needing real help. ‘Oh, you’re catastrophizing?’ No, I’m in a wheelchair because my spine is collapsing. Your thought record won’t fix that.
Stop romanticizing cognitive restructuring. It’s not a cure. It’s a band-aid on a hemorrhage.
Alicia Hasö
January 16, 2026 at 02:33Heather, I hear you. And I’ve been there. I’ve sat in waiting rooms for months, begging for an MRI, praying for a surgeon who’d say, ‘We can fix this.’
But here’s what no one tells you: even when your body is broken, your mind can still choose how much power it gives the pain.
I had a spinal fusion. It helped. But I still had the same fear-the same terror that every ache meant another collapse. CBT didn’t change my spine. It changed how I breathed through the fear.
And guess what? I started gardening again. I held my niece for the first time without crying. I didn’t need a miracle. I needed to stop letting my thoughts steal my moments.
This isn’t about replacing medicine. It’s about giving people tools when medicine alone isn’t enough. And for so many of us? It’s the only thing that lets us feel human again.
Matthew Maxwell
January 16, 2026 at 20:55Anyone who says CBT works for chronic pain is either delusional or paid by Big Pharma to push non-pharmaceutical alternatives.
Let’s not pretend this is science. It’s positive thinking with a fancy acronym. If your pain is real, no amount of ‘5-4-3-2-1’ is going to undo nerve damage.
And don’t even get me started on the VA pushing this. They’re cutting opioid prescriptions and replacing them with worksheets. That’s not healthcare. That’s austerity dressed up as empowerment.
Real pain doesn’t care about your thought records. It doesn’t care if you ‘re-frame’ it. It just hurts. And if you’re telling people to ‘just breathe’ instead of giving them real relief-you’re part of the problem.
Jeffrey Hu
January 17, 2026 at 19:03Wow. So you’re telling me I just need to ‘challenge my thoughts’ instead of getting a nerve block? That’s rich.
Let me guess-your pain is ‘manageable’ and you’ve never had to sit through 18 hours of epidural steroid injections because your doctor said ‘try CBT first.’
There’s a reason people call this ‘the therapy for people who can’t afford real treatment.’
And the fact that you’re calling it ‘science-backed’ while ignoring the 70% of chronic pain patients who don’t respond to CBT? That’s not evidence. That’s propaganda.
Elisha Muwanga
January 18, 2026 at 15:34It’s not about whether the pain is real. It’s about whether you’re willing to stop letting your mind run the show. I’ve had both. I’ve had the surgery. I’ve had the meds. I’ve had the CBT. And only CBT gave me back my life. Not because it erased the pain-but because it stopped me from letting it erase me.
Pooja Kumari
January 20, 2026 at 04:39I’ve been doing this for 8 years. I used to cry every morning before I even opened my eyes. I thought I was broken beyond repair. I thought I’d never laugh again. Then I started writing down my thoughts-just one a day. Not because I believed it. Just because I was tired of being a prisoner in my own head.
Some days I wrote: ‘I hate this.’ That’s it. Just that.
Other days I wrote: ‘I walked to the mailbox. It hurt. But I did it.’
It didn’t fix my pain. But it gave me back my voice. And for someone who spent years feeling invisible? That was everything.
I’m not ‘cured.’ I’m not ‘fixed.’ But I’m here. And I’m not letting fear steal another day.
If you’re reading this and you’re still in bed, wondering if you’re weak for still hurting… you’re not weak. You’re surviving. And that’s enough.