Every year, over 1.3 million people in the U.S. end up in the emergency room because of problems with their medications. Many of these cases aren’t caused by bad drugs or careless doctors-they’re caused by habits that make medications less safe, or even unnecessary. The truth is, you don’t always need more pills to stay healthy. Sometimes, you just need to change how you live.
Why Lifestyle Changes Matter More Than You Think
Taking multiple medications-known as polypharmacy-is common, especially as we get older. But if you’re on five or more drugs, your risk of dangerous side effects jumps by 300%. That’s not just a number. It means more falls, more confusion, more hospital visits. And often, those medications are treating symptoms, not the real cause. Lifestyle changes don’t replace medicine. They make medicine work better. A 2023 study of over 3.4 million people found that people who improved their diet, moved more, and slept better reduced their need for medication by 25% to 50% for conditions like high blood pressure, diabetes, and high cholesterol. That’s not a guess. That’s science. You might think, “I’m already taking my pills, why bother?” But here’s the catch: if you’re eating junk food, sitting all day, and sleeping poorly, your body isn’t responding the way it should. Medications can’t fix a broken foundation. Lifestyle changes fix the foundation.Move More-Even a Little
You don’t need to run marathons. You don’t need a gym membership. Just move. JenCare Medical Centers found that walking briskly for 30 minutes, three days a week, can lower blood pressure as effectively as a first-line blood pressure pill. Why? Because walking makes your heart stronger. A stronger heart doesn’t have to work as hard. That means less pressure on your arteries-and less need for medication. For people with type 2 diabetes, movement helps your muscles use glucose without insulin. A 5% to 7% drop in body weight from regular activity can cut diabetes medication needs by up to 60% in prediabetes and 40% in those already diagnosed. That’s not magic. That’s biology. The American Heart Association recommends 150 minutes of moderate exercise each week. That’s 30 minutes, five days a week. If that feels too much, start with 10 minutes a day. Build up. The goal isn’t perfection-it’s consistency.Eat to Support Your Meds, Not Fight Them
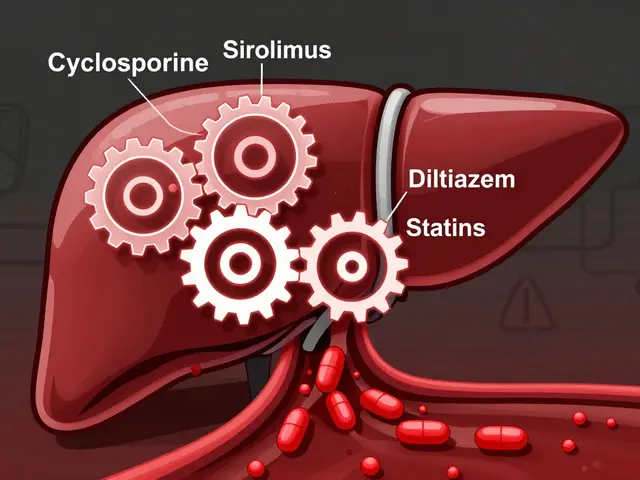
Food isn’t just fuel. It’s medicine. But some foods can interfere with your pills. Grapefruit, for example, affects 85% of statins-the drugs used to lower cholesterol. Eating just half a grapefruit can cause your body to absorb too much of the drug, leading to muscle damage or kidney problems. If you’re on a statin, skip the grapefruit. Simple. If you’re taking warfarin (a blood thinner), watch your leafy greens. Spinach, kale, and broccoli are full of vitamin K, which works against warfarin. You don’t have to avoid them-just eat them the same amount every day. Consistency is key. Dairy products can block the absorption of certain antibiotics. Don’t take your pill with milk. Wait two hours before or after. For high blood pressure, cutting sodium is as powerful as a pill. The DASH diet (Dietary Approaches to Stop Hypertension) cuts sodium to under 1,500 mg a day and focuses on fruits, vegetables, whole grains, and lean protein. Studies show it can lower blood pressure by 11/5 mm Hg-same as one medication. For type 2 diabetes, a diet low in refined carbs and sugar can bring blood sugar down as much as metformin. It’s not about starving. It’s about swapping white bread for whole grain, soda for water, candy for fruit.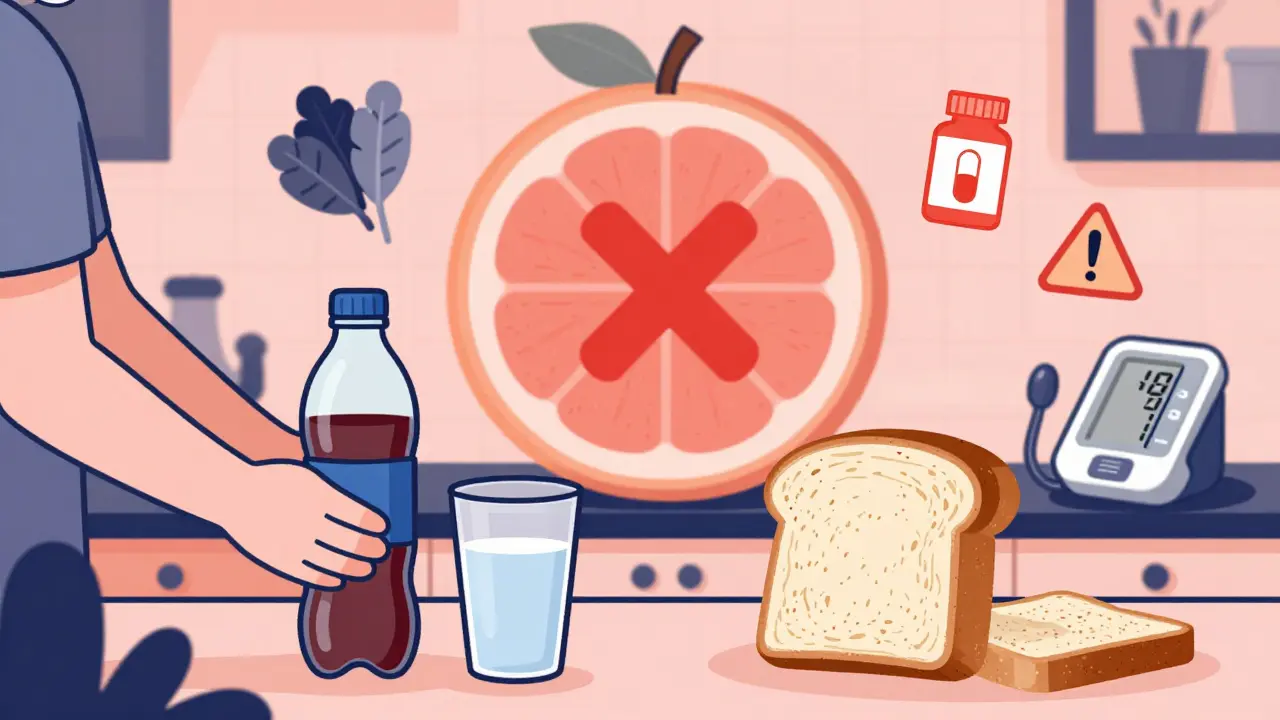
Sleep Like Your Life Depends on It-Because It Does
You’ve heard it before: sleep is important. But here’s the real impact: if you regularly get less than seven hours of sleep, your risk of high blood pressure, diabetes, and obesity goes up. And those conditions? They’re the exact reasons you’re on medication. Poor sleep makes your body less sensitive to insulin. That means your blood sugar stays high, even if you’re taking pills. It also raises stress hormones like cortisol, which spikes blood pressure. Aim for seven to nine hours every night. That means turning off screens an hour before bed, keeping your room cool and dark, and going to bed and waking up at the same time-even on weekends. If you’re snoring loudly or waking up tired, you might have sleep apnea. That’s not just annoying-it’s dangerous. It raises your risk of heart attack and stroke. Talk to your doctor. A simple sleep test can change your life.Quit Smoking, Cut Alcohol, Manage Stress
Smoking isn’t just bad for your lungs. It makes your blood pressure rise, your arteries stiffen, and your heart work harder. If you’re on blood pressure or heart meds, smoking makes them less effective. Quitting can lower your blood pressure within weeks. Alcohol? Limit it. For men, no more than two drinks a day. For women, one. More than that raises blood pressure, interferes with liver function (where many drugs are processed), and increases the risk of falls and confusion, especially in older adults. Stress is silent poison. It raises cortisol, spikes blood sugar, and tightens blood vessels. Yoga, meditation, deep breathing-even 10 minutes a day-can lower blood pressure and reduce anxiety. You don’t need to be a monk. Just pause. Breathe. Reset.Work With Your Doctor-Don’t Go It Alone
Never stop or change your meds on your own. Even if you feel better, your body might still need the drug. Stopping suddenly can cause rebound high blood pressure, seizures, or heart problems. Instead, talk to your doctor about your lifestyle changes. Bring your progress: your step count, your food log, your sleep tracker. Ask: “Can we re-evaluate my meds in three months?” Pharmacists are your secret weapon. They know which foods interact with which drugs. Ask them during your next refill. “Is it safe to eat grapefruit with this?” “Can I take this with dairy?” Simple questions. Big answers. Some clinics now offer lifestyle medicine programs-certified by the American College of Lifestyle Medicine. These aren’t vague “eat better” advice. They’re structured plans with tracking, coaching, and medical oversight. Ask your doctor if one is available.




Jody Fahrenkrug
January 16, 2026 at 11:50Been doing the 30-min walk thing 3x a week since January. My BP dropped from 142/90 to 128/82. Didn’t even touch my meds. Just moved more. Weird how simple stuff works when you stop overcomplicating it.
Also stopped drinking soda. Switched to sparkling water with lime. My sugar cravings? Gone. No magic, just consistency.
Samyak Shertok
January 16, 2026 at 21:10Oh wow. So the solution to 1.3 million ER visits is… walking? And not eating grapefruit? Did we skip the part where Big Pharma stopped lying to us? I’m sure the FDA just forgot to mention that ‘exercise’ is cheaper than a statin.
Next they’ll tell us breathing is a cure for cancer. Oh wait-someone already wrote a TED Talk about that. And got a sponsorship from Peloton.
Stephen Tulloch
January 18, 2026 at 16:43LMAO at the ‘walk 30 minutes’ advice. I’m 68 and have three knee replacements. You think I don’t know movement helps? I’ve been doing tai chi since 2010. But my doctor still gave me 7 prescriptions because ‘your numbers are off.’
Meanwhile, my neighbor’s on 11 meds and walks 2 miles daily. Guess who’s in the ER last month? Him. Not me. Lifestyle doesn’t fix broken systems. It just makes you feel guilty for being human.
Also, grapefruit? Bro I’ve been eating it with my statin for 8 years. Still standing. 🍊💪
Joie Cregin
January 20, 2026 at 16:14Y’all are underestimating how hard this stuff is. Like… I get the science. I’ve read the studies. But when you’re exhausted from working two jobs, raising kids, and your partner doesn’t get it? Trying to eat clean feels like climbing Everest in flip-flops.
I started with one thing: swapping my 3pm soda for herbal tea. Just that. And now I don’t crave sugar as much. It’s not perfect. But it’s mine. And I’m proud.
To anyone struggling: tiny wins count. You’re not failing. You’re showing up. That’s enough. 🌱💛
Rob Deneke
January 21, 2026 at 10:16Just started walking after dinner. 15 minutes. No fancy shoes. Just my slippers. My wife says I look like a confused penguin but I feel better already. No more afternoon crashes. Sleep’s deeper too. Keep it simple. Just move. One step at a time
Also stop eating chips before bed. Your body doesn’t care if it’s ‘low sodium’ it still hates it
Chelsea Harton
January 21, 2026 at 21:04sleep fixes everything
once i stopped scrolling at 1am my bp dropped
no joke
also grapefruit is a trap
why is it even a thing
waneta rozwan
January 23, 2026 at 19:19Oh so now it’s our fault we’re on meds? We’re lazy? We don’t care? Newsflash: I’ve been doing yoga, eating organic, and sleeping 8 hours since 2018. And I’m still on 5 pills because my body doesn’t care about your ‘lifestyle’ Instagram post.
Stop gaslighting people with chronic illness. Not everyone can afford kale. Not everyone can walk. Not everyone’s body responds to ‘just move more.’
This article is dangerously naive. And I’m tired of it.
Kasey Summerer
January 24, 2026 at 23:01So the American Heart Association says 68% felt better after lifestyle changes... but only 32% said it was too hard? Bro that’s not a success rate, that’s a cultural indictment.
Meanwhile in India, my cousin takes 8 meds and eats fried samosas every morning. He’s 84. Still plays cricket. No hospital visits. Maybe the real problem isn’t the diet… it’s the obsession with ‘optimizing’ everything.
Maybe we just need to chill. And eat more curry. 🇮🇳✌️