Every year, over 51 million medication errors happen in U.S. community pharmacies. Most of these aren’t caught by barcode scanners or double-check systems. But there’s one moment - right before the patient walks out - where the error can still be stopped. That moment is patient counseling.
Why Patient Counseling Is the Last Line of Defense
Patient counseling isn’t just about telling someone how to take their pills. It’s the final safety net. According to Pharmacy Times, 83% of dispensing errors are caught during these brief conversations. That’s higher than barcode scanning (53%) or pharmacist double-checks (67%). Why? Because machines can’t ask, “Does this look right to you?” or “What’s this for?” Patients can. When a patient says, “I’ve never taken a blue pill before,” or “My last one was bigger,” that’s not just feedback - it’s a red flag. The Institute for Safe Medication Practices calls this a “human firewall.” No automated system can replace a patient’s real-world experience with their own medication.The Four Critical Checks Every Pharmacist Must Do
Effective counseling isn’t random. It follows a proven structure. The American Pharmacists Association recommends four key steps, each with a specific purpose:- Verify identity and medication purpose - Ask: “What condition is this medication for?” Don’t assume. A patient might say “for my knee,” but the script says “for gout.” That mismatch is a red flag.
- Check how they’ll take it - Use the “teach-back” method. Ask them to show you how they’ll take it. If they say, “I’ll crush it and mix it with applesauce,” but the label says “swallow whole,” you’ve caught a dangerous mistake.
- Confirm the physical appearance - Show the patient the pill or liquid. Ask, “Does this look like what you’ve taken before?” This catches look-alike errors - like confusing insulin vials or confusing 10mg and 50mg tablets. Studies show this step alone catches 29% of these errors.
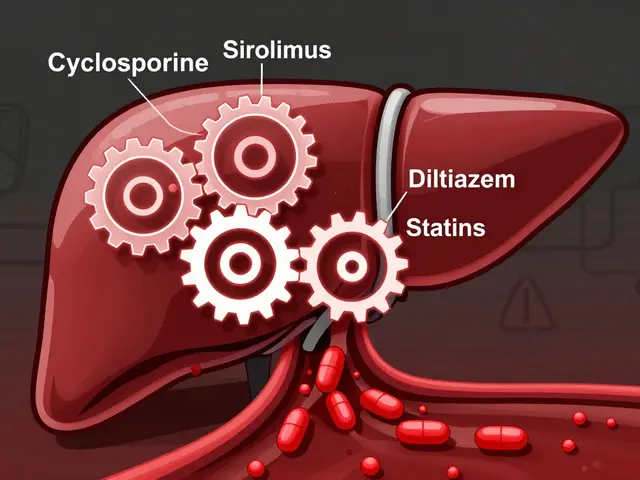
- Review interactions and allergies - Cross-check their current meds. Did they just start a new blood thinner? Are they allergic to sulfa? Don’t just read the screen - ask, “Have you had any bad reactions to meds in the past?”
Each step takes time. Research shows you need at least 2.3 minutes per patient to catch most errors. Shorter sessions - under 90 seconds - cut detection rates by nearly half.
Open Questions Beat Yes/No Questions
The way you ask matters more than you think. Closed questions like “Is this for your blood pressure?” often get a “yes” even when the patient isn’t sure. Open questions like “What do you understand this medication is for?” reveal confusion. Pharmacy Times found open-ended questions identify 3.2 times more errors than yes/no questions. Why? Because patients often don’t know what they don’t know. When you give them space to explain, gaps show up. A real example: A patient was given metformin but thought it was for “diabetes sugar.” When asked to explain, they said, “I take it when I feel dizzy.” That’s not how metformin works. The pharmacist caught a wrong indication - and a potential misdiagnosis.
Who Needs Counseling the Most?
Not all patients are equally at risk. The highest-risk groups are:- Patients over 65 - dosing errors here are 3.7 times more likely to cause serious harm.
- People with low health literacy - they make up 42% of undetected errors because they won’t admit they don’t understand.
- Those starting new high-alert medications - insulin, opioids, warfarin, or chemotherapy drugs. The ISMP says 1 in 5 errors involve these.
- Patients on five or more medications - complex regimens increase error risk by 70%.
For these patients, counseling isn’t optional. It’s a safety requirement. The Joint Commission’s 2022 guidelines specifically say: “Engage patients as partners in safety.” That means tailoring your approach to those most at risk.
What Happens When Counseling Is Rushed?
In many chain pharmacies, pharmacists are expected to fill 14+ prescriptions per hour. That’s less than 4 minutes per script - including labeling, checking, and counseling. Real data from the University of Arizona shows: when pharmacists hit that pace, counseling error detection drops from 83% to 41%. At CVS, technicians reported spending only 1.2 minutes per counseling session on average. That’s half the recommended time. And in Reddit’s r/pharmacy community, pharmacists say they’re told not to “slow down the line.” But here’s the catch: when counseling is rushed, errors slip through - and patients get hurt. One patient in a Healthgrades review wrote: “The pharmacist caught that my new blood thinner was the wrong strength when I said it looked smaller than before.” That’s the kind of moment that saves lives. But it only happens if you take the time.Cost vs. Benefit: Why Counseling Pays Off
Some pharmacies see counseling as a cost. It takes time. It slows things down. But here’s the real math:- Cost per counseling session: $0.87
- Cost per barcode scan: $1.35
- Cost per pharmacist double-check: $2.10
That’s not just cheaper - it’s more effective. Independent pharmacies that use structured counseling report a 19% drop in malpractice insurance premiums. Why? Fewer errors mean fewer lawsuits.
CMS now ties 8.5% of Medicare Part D reimbursement to documented counseling that includes error verification. And according to Evaluate Pharma, pharmacies with strong counseling protocols will gain 12-15% more market share by 2027 - because patients choose them. A 2023 NCPA survey found 83% of patients prefer pharmacies where pharmacists take time to explain meds.
How to Make Counseling Work in Your Pharmacy
If you want to improve error detection, here’s what works:- Train your team - Use APhA’s 4-step framework. Practice teach-back with role-playing.
- Use pharmacy technicians - In 42 states, techs can do preliminary counseling. They can verify purpose and appearance, freeing pharmacists to focus on interactions and allergies.
- Document everything - Use NABP’s 2022 standards. Note what was discussed, what the patient said, and any corrections made. This cuts liability claims by 44%.
- Start with high-risk scripts - Prioritize new prescriptions, opioids, insulin, and complex regimens. Don’t try to counsel every refill the same way.
- Track your numbers - How many errors did you catch last month? How many patients said, “I thought this was different”? Use that data to improve.
One pharmacy in Michigan implemented the full 4-step protocol. Within six months, their error detection rate jumped from 61% to 85%. That’s not luck. That’s process.
The Future of Counseling: Tech That Helps, Not Replaces
New tools are emerging. Surescripts’ 2024 “Counseling Checkpoint” API lets pharmacists log verification steps right in their workflow software. Early adopters say it cuts time by 22% without lowering accuracy. The FDA says patient counseling remains the most effective way to catch errors that technology misses - especially for compounded medications, where error rates are nearly five times higher. But no app will ever replace a patient saying, “This doesn’t look right.” That’s why the American Society of Health-System Pharmacists is aiming to raise detection rates from 83% to 90% by 2025 - not by adding more tech, but by improving how we talk to patients.How long should a patient counseling session last to catch dispensing errors?
Research shows you need at least 2.3 minutes per patient to catch the majority of dispensing errors. Each additional 30 seconds increases detection rates by 12.7%. Sessions under 90 seconds reduce error detection by nearly half. The recommended full protocol - including identity, purpose, appearance, and interaction checks - takes about 2 minutes and 40 seconds.
Can pharmacy technicians help with patient counseling for error detection?
Yes. In 42 U.S. states, pharmacy technicians are legally allowed to perform preliminary counseling - verifying the patient’s name, medication purpose, and physical appearance. This frees pharmacists to focus on complex interactions, allergies, and patient understanding. When used correctly, technician involvement can increase effective counseling time by 37%.
What’s the most common type of dispensing error caught during counseling?
The most common error caught is a mismatch between the medication’s intended use and the patient’s understanding. For example, a patient is given metformin for diabetes but believes it’s for “low energy.” Other frequent catches include wrong strength (e.g., 10mg instead of 50mg), wrong formulation (tablet vs. capsule), and look-alike medications like confusing insulin types. About 29% of look-alike errors are caught when patients are asked if the pill looks familiar.
Why is patient counseling more effective than barcode scanning?
Barcode scanning verifies the right drug, dose, and patient - but it can’t detect if the prescription was written for the wrong condition, if the patient misunderstands how to take it, or if the pill looks different than expected. Counseling catches the human element: confusion, assumptions, and miscommunication. That’s why it catches 83% of errors compared to 53% for barcode systems.
Do patients actually want thorough counseling?
Yes. A 2023 analysis of 1,247 patient reviews on Healthgrades and Yelp found 89% appreciated thorough counseling that caught potential errors. One patient wrote: “The pharmacist caught that my new blood thinner was the wrong strength when I said it looked smaller than before.” Only 11% complained about delays - and most of those were from people who didn’t realize the safety benefit.


Francine Phillips
December 3, 2025 at 14:15This whole post is overkill. I’ve worked in a pharmacy for 12 years and never once had a patient catch an error because they said the pill looked different.
Makenzie Keely
December 4, 2025 at 09:51Actually, that’s exactly the point-patients *do* catch errors, and when they don’t, it’s because we’re rushing them out the door. I’ve had patients say, ‘This isn’t the same blue pill I got last month,’ and it turned out to be a wrong strength. We’ve got the data: 83% of errors caught during counseling. That’s not luck-it’s a system. Stop treating patients like obstacles in the workflow.
And yes, it takes time. 2.3 minutes minimum. But if you’re doing 14 scripts an hour, you’re not a pharmacist-you’re a pill dispenser. The Joint Commission isn’t joking when they say patients are safety partners. We’re not doing them a favor by talking to them-we’re saving their lives.
Also, technicians can and should do the first three steps: verify identity, purpose, and appearance. That frees pharmacists to focus on interactions and allergies. It’s legal in 42 states. Stop pretending we don’t have the tools.
And don’t even get me started on the ‘but it slows us down’ excuse. The cost per counseling session is $0.87. The cost per malpractice claim? $120,000. The math isn’t even close.
And yes, I’ve documented every single counseling session since 2020 using NABP standards. My insurance premium dropped 19%. My patients now ask for me by name. That’s not ‘nice’-that’s business.
And before you say ‘patients don’t care’-check the Healthgrades reviews. 89% of them thanked us for catching errors. Only 11% complained about wait time-and most of those didn’t even know why we were asking questions.
It’s not about being ‘nice.’ It’s about being competent. And if you’re not doing this, you’re not doing your job.
bobby chandra
December 4, 2025 at 20:15Let’s be real-this isn’t just about safety, it’s about branding. Patients remember the pharmacist who asked, ‘What do you think this is for?’ They don’t remember the one who handed them a script and said ‘Take two.’ We’re not just filling prescriptions-we’re building trust. And trust = loyalty = more business. The NCPA survey says 83% of patients pick pharmacies where they feel heard. That’s not fluff-that’s profit.
And the tech? Surescripts’ Counseling Checkpoint API? Game-changer. It logs everything in real time without adding steps. We rolled it out last month. Our average counseling time went from 1:48 to 2:42. Error detection jumped from 68% to 87%. No extra staff. No extra cost. Just better workflow.
Stop thinking of counseling as overhead. Think of it as your competitive advantage.
Katherine Gianelli
December 6, 2025 at 17:13I’ve been a caregiver for my mom for years and I’ve seen it all-the wrong insulin vial, the crushed pills mixed into applesauce, the confusion between ‘for pain’ and ‘for inflammation.’ One time she took a new blood pressure med because the pill looked like the old one-except it was twice the dose. We almost lost her.
That’s why I scream at every pharmacist who rushes me: ‘Ask me what this is for!’ I don’t care if you’ve got a line out the door-I care that my mom doesn’t end up in the ER because someone didn’t ask the right question.
And don’t tell me she’s ‘not articulate.’ She’s 79, has low health literacy, and doesn’t trust doctors anymore. But she’ll tell you if the pill looks different. She’ll say, ‘This one’s not yellow.’ That’s not a flaw-that’s a superpower.
We need to stop blaming patients for not knowing medicine. We need to stop assuming they’re lying when they say, ‘I’ve never taken this before.’ We need to stop treating them like they’re a burden.
They’re the last line of defense. And if we don’t treat them like it, we’re not just failing them-we’re failing ourselves.
vinoth kumar
December 6, 2025 at 17:29Love this! In India, we don’t have barcode scanners everywhere, but we still catch errors by asking patients-‘Did you get this before?’ or ‘What did the doctor say this is for?’ It works. Simple. Human. I’ve had patients catch wrong doses because they remembered their last bottle had a different shape.
Also, I train my techs to do the first three steps-name, purpose, appearance. Saves so much time. And patients feel respected. They say ‘thank you’ more than ‘hurry up.’
Maybe US pharmacies need less tech and more heart.
Gene Linetsky
December 7, 2025 at 14:27Let’s be honest-this whole ‘patient counseling’ thing is just corporate propaganda. The real reason they’re pushing it is because insurance companies want to reduce claims. And now they’re forcing pharmacists to do more paperwork under the guise of ‘safety.’
Barcodes work fine. Double-checks work fine. Patients don’t know what they’re taking half the time-they’re just happy to get their meds. If they say ‘this looks different,’ it’s probably just a generic switch. Stop making patients feel like they’re detectives.
And don’t even get me started on the ‘83% error detection’ stat. Where’s the peer-reviewed study? Sounds like a marketing slide from a pharmacy tech startup.
Meanwhile, real pharmacists are burned out, underpaid, and forced to do 14 scripts an hour while being yelled at by patients who think they’re magicians. This post is just guilt-tripping us into working harder for less.
Ignacio Pacheco
December 9, 2025 at 01:24So let me get this straight-we’re supposed to believe that a 78-year-old woman with three chronic conditions and no clue what metformin is, is somehow better at catching a dosing error than a machine that scans barcodes, checks allergies, and verifies the prescriber?
That’s not a ‘human firewall.’ That’s a statistical outlier wrapped in emotional storytelling.
And yet somehow, the post ignores the fact that most patients don’t even remember what meds they’re on. Half the time, they say ‘it’s for my heart’ when it’s for diabetes. The ‘teach-back’ method? Great in theory. In practice? Most patients just nod and say ‘yes’ because they’re embarrassed.
So we’re supposed to trust the one person in the room who has zero medical training, is probably confused, and is just trying to get out the door? That’s not safety. That’s desperation dressed up as empathy.
Also, 2.3 minutes per patient? That’s not counseling. That’s a therapy session. Who’s paying for that? The patient? The pharmacy? The government? Nobody wants to pay for it. So it’s just a nice-sounding ideal that no one can afford.
Archie singh
December 10, 2025 at 21:45Wow. Another sanctimonious rant from someone who thinks they’re the only pharmacist who’s ever cared about patients. Let me guess-you also cry when you see a patient holding their meds and say ‘I hope they don’t die.’
Newsflash: Patients don’t care about your 4-step framework. They care if their prescription is ready. They don’t want to explain their ‘gout’ to you. They don’t care that your ‘teach-back’ method is ‘evidence-based.’
And you think your 83% error detection rate is because of ‘counseling’? Or is it because you’re the only one who actually reads the script? Maybe you’re just better at your job.
Stop pretending this is about patients. It’s about liability. It’s about insurance. It’s about avoiding lawsuits. And now you’re weaponizing guilt to make pharmacists feel bad for not doing 10x more work for the same pay.
And yes-I’ve seen patients lie about allergies. I’ve seen them say ‘yes’ to everything because they’re scared you’ll yell at them. So your ‘human firewall’? It’s a sieve.
Real solution? Better training. Better systems. Not more talking.