REM sleep behavior disorder isn’t just about dreaming loudly or kicking in your sleep. It’s a warning sign your brain is changing in ways that could lead to Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy. If you or your partner have noticed you’re acting out dreams-shouting, punching, jumping out of bed-you’re not just having bad dreams. You’re experiencing a neurological red flag.
What Exactly Is REM Sleep Behavior Disorder?
During normal REM sleep, your body is temporarily paralyzed. This is called muscle atonia. It keeps you from physically acting out your dreams. In REM sleep behavior disorder (RBD), that paralysis fails. Your muscles stay active. You might yell, flail, kick, or even get out of bed and run into walls. These episodes usually happen in the second half of the night, when REM sleep is longest and most intense.It’s not just disruptive-it’s dangerous. Studies show 78% of people with RBD make changes to their bedroom to avoid injury: removing sharp furniture, installing bed rails, taking weapons out of the room. One in two patients eventually sleep separately from their partner because of the risk.
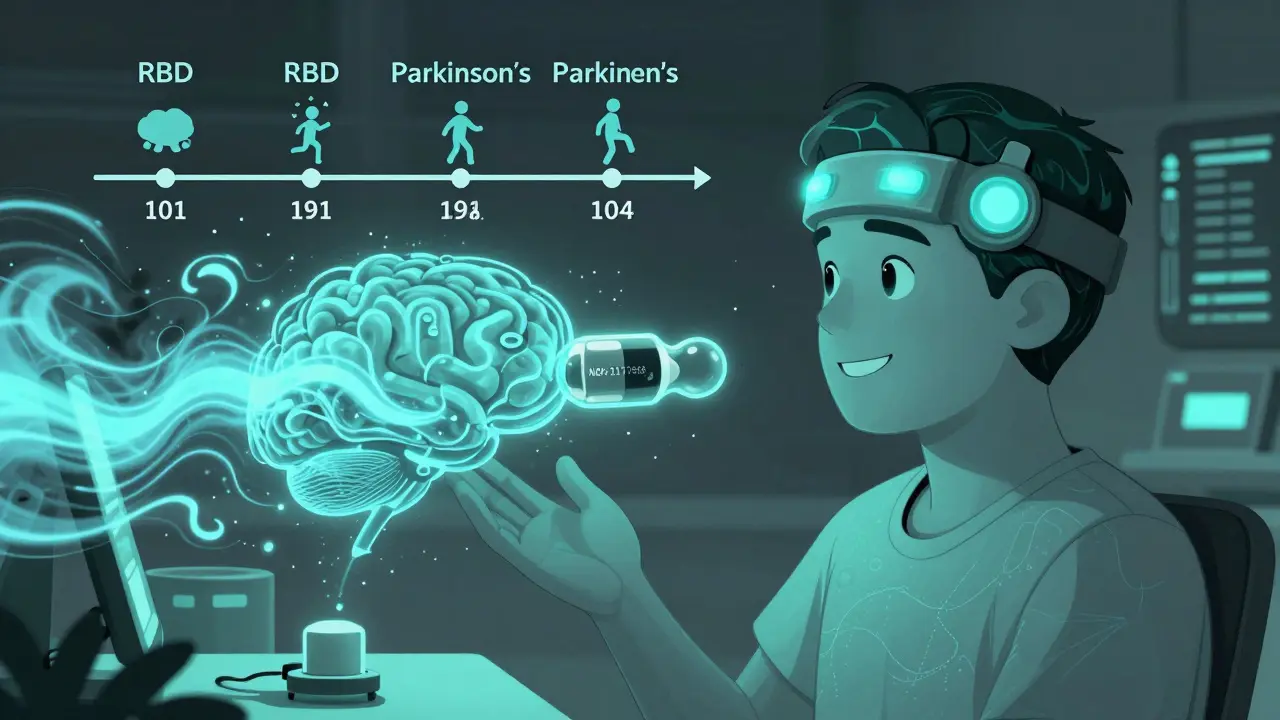
What makes RBD especially concerning is that it’s often the first sign of a neurodegenerative disease. About 73.5% of people with idiopathic RBD (meaning no known cause) develop Parkinson’s, dementia with Lewy bodies, or multiple system atrophy within 12 years. That’s why diagnosing RBD isn’t just about helping you sleep better-it’s about catching a brain disease before it fully takes hold.
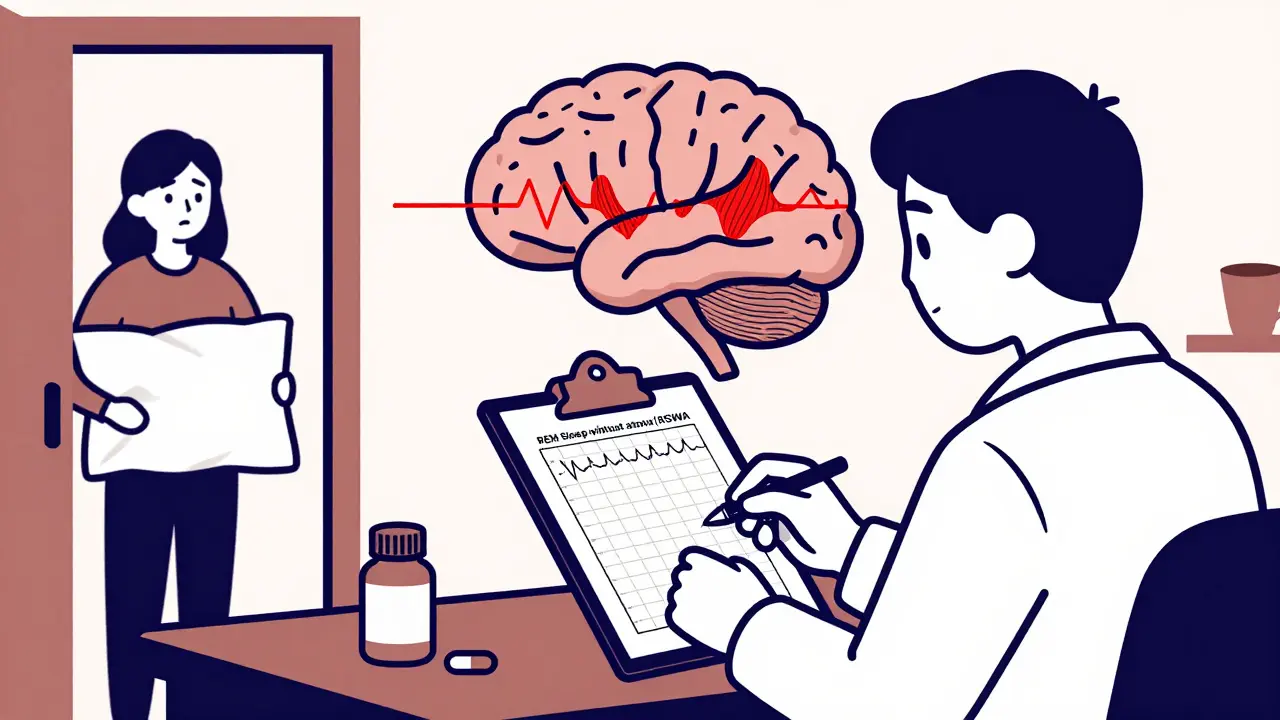
How Is RBD Diagnosed?
You can’t diagnose RBD by just describing symptoms. You need a sleep study-polysomnography (PSG). This test records brain waves, eye movements, heart rate, breathing, and muscle activity while you sleep.The key finding? REM sleep without atonia (RSWA). That means your muscles are moving during REM sleep when they shouldn’t be. The International Classification of Sleep Disorders requires that at least 15% of REM sleep epochs show abnormal muscle activity. In many cases, patients have complex movements averaging 4.2 times per hour.
Doctors also look for other clues: did the behavior start after age 50? Is there a history of head trauma or narcolepsy? Are you taking antidepressants? Some medications can trigger RBD-like symptoms. But if you’re over 50, have no clear trigger, and your sleep study shows RSWA, the odds are high this is idiopathic RBD-and a sign of future neurodegeneration.
First-Line Treatments: Melatonin and Clonazepam
There are no FDA-approved drugs specifically for RBD. Treatment is off-label, based on decades of clinical experience and small trials. Two medications stand out: melatonin and clonazepam.Melatonin is a natural hormone that helps regulate sleep-wake cycles. For RBD, it’s used in doses of 3 to 12 mg at bedtime. A 2010 randomized trial found 62.5% of patients had fewer dream enactment episodes. More recent data from the Cleveland Clinic shows some patients go from seven episodes a week to just one after starting 6 mg nightly. Side effects are mild-headache, dizziness, morning grogginess-and affect only about 8% of users.
Clonazepam, a benzodiazepine, has been the go-to for decades. It works by enhancing GABA, a calming brain chemical that suppresses muscle activity. Studies show it reduces symptoms in 80-90% of patients. One 2000 study reported 88.7% effectiveness. Many patients feel better within days. But it’s not without risk. Side effects include dizziness (22%), unsteadiness (18%), and daytime sleepiness (15%). For older adults, the risk of falls increases by 34%. Long-term use can lead to dependence, tolerance, and withdrawal nightmares if stopped suddenly.
Today, 58% of neurologists start with melatonin. Only 32% begin with clonazepam. Why? Safety. Melatonin doesn’t cause falls, addiction, or cognitive fog. It’s especially preferred for older patients or those with balance issues.
Other Medications and Emerging Options
For patients who don’t respond to melatonin or clonazepam, doctors may try other options:- Pramipexole (a dopamine agonist used for Parkinson’s and restless legs syndrome) helps about 60% of patients, especially those with coexisting RLS. Dose: 0.125-0.5 mg daily.
- Rivastigmine (an Alzheimer’s drug) showed promise in a single trial for RBD patients with mild cognitive impairment. It’s not widely used, but may help when other treatments fail.
The most exciting development? Dual orexin receptor antagonists. Orexin is a brain chemical that keeps you awake. Blocking both orexin receptors (Ox1 and Ox2) may calm the overactive brain circuits driving RBD. Mount Sinai’s 2023 research showed a 78% reduction in dream enactment in animal models. Suvorexant (Belsomra), already FDA-approved for insomnia, is being tested for RBD. Neurocrine Biosciences’ drug NBI-1117568 received Fast Track designation from the FDA in January 2023. Phase II trials are underway, with results expected in 2024.
These new drugs could offer the same effectiveness as clonazepam without the risk of falls, dependence, or cognitive decline. They’re not available yet-but they’re coming.
Neurological Monitoring: It’s Not Just About Sleep
If you have RBD, your brain is already on a path toward neurodegeneration. The American Academy of Neurology recommends annual neurological exams for all patients with idiopathic RBD. Why? Because the conversion rate to Parkinson’s or dementia is about 6.3% per year.During these check-ups, doctors look for early signs: subtle changes in smell, constipation, REM sleep without atonia worsening, mild tremors, or reduced arm swing while walking. These aren’t symptoms you’d notice on your own-but they’re clues.
Some patients are now enrolled in research studies tracking biomarkers: alpha-synuclein levels in spinal fluid, brain imaging for dopamine loss, or changes in eye movement patterns. The goal? To find a way to stop the disease before it causes memory loss or movement problems.
Non-Drug Strategies: Safety Comes First
Medication helps-but it doesn’t eliminate risk. That’s why safety steps are just as important.- Remove all weapons, sharp objects, and glass from the bedroom.
- Pad sharp corners of furniture.
- Place thick rugs or mats beside the bed.
- Install bed rails or use a mattress on the floor.
- Avoid alcohol. Even one or two drinks can trigger an episode in 65% of patients.
- Don’t sleep in a bunk bed or top bunk.
Many couples report dramatic improvements after these changes-even before starting medication. One spouse said, “After my husband started 0.5 mg clonazepam, I could finally sleep in the same bed without fear of being kicked or punched.”
What Happens If You Don’t Treat It?
Left untreated, RBD doesn’t just hurt your sleep-it hurts your life. Injuries are common: bruises, broken bones, concussions. Relationships suffer. Partners report chronic sleep deprivation, anxiety, and fear. Many end up sleeping in separate rooms.But the bigger risk? Missing the window to intervene in neurodegeneration. By the time Parkinson’s or dementia symptoms appear, brain damage is often advanced. RBD gives you a 10-15 year head start. That’s time to monitor, prepare, and potentially join clinical trials for disease-modifying therapies.
When to See a Specialist
If you or your partner notice any of these:- Acting out dreams (shouting, punching, kicking)
- Injuries during sleep
- Waking up confused or sore with no memory of the event
- Starting these behaviors after age 50
See a sleep specialist or neurologist. Get a polysomnogram. Don’t wait. RBD is one of the strongest predictors of future neurodegenerative disease-and early detection is your best defense.
What’s Next?
The next five years will likely bring the first treatments that don’t just calm your dreams-but slow or stop the brain changes behind them. Until then, melatonin and safety measures are your best tools. Clonazepam works, but its risks make it a second choice for many. Stay informed. Track your symptoms. And don’t ignore the warning signs. Your brain is speaking. Listen.Can REM sleep behavior disorder be cured?
There’s no cure for RBD yet. Current treatments manage symptoms but don’t stop the underlying brain changes. About 73.5% of people with idiopathic RBD eventually develop Parkinson’s, dementia with Lewy bodies, or multiple system atrophy. The focus now is on early detection and slowing progression. New drugs targeting the root cause are in development, with clinical trials expected to yield results by 2025.
Is melatonin safe for long-term use in RBD?
Yes. Melatonin is one of the safest options for long-term use in RBD. Studies show only 8% of users report mild side effects like headache or morning grogginess. Unlike clonazepam, it doesn’t cause dependence, falls, or cognitive decline. Doses up to 12 mg nightly have been used safely for years in older adults. It’s the preferred first-line treatment for patients over 65 or those with balance issues.
Why is clonazepam still used if it has so many side effects?
Clonazepam works quickly and effectively-80-90% of patients see improvement within days. For patients who don’t respond to melatonin, or who have severe, dangerous episodes, the benefits often outweigh the risks. But because of fall risk, dependence, and daytime drowsiness, it’s no longer the first choice. It’s reserved for cases where safety is urgently at risk and melatonin failed.
Can alcohol make REM sleep behavior disorder worse?
Yes. Even one or two alcoholic drinks can trigger or worsen RBD episodes in 65% of patients. Alcohol disrupts normal sleep architecture and reduces muscle atonia during REM sleep. Avoiding alcohol entirely is one of the most effective non-medication strategies for reducing episodes. This applies even if you’re taking medication.
Should I get a brain scan if I have RBD?
Routine brain scans like MRI or CT aren’t needed for diagnosis. But specialized imaging-like dopamine transporter scans (DaTscan)-can help predict progression to Parkinson’s. These scans are used in research and specialized clinics. If you’re being monitored for neurodegeneration, your neurologist may recommend one to track dopamine loss over time.
Can RBD develop in younger people?
Yes, but it’s rare. Most cases start after age 50. In younger patients, RBD is often linked to other conditions: narcolepsy, antidepressant use (especially SSRIs), or brain injury. If you’re under 50 and have RBD, your doctor will look for these triggers. The risk of developing Parkinson’s or dementia is much lower in younger patients with secondary RBD compared to those with idiopathic RBD over 60.
Are there any new drugs coming for RBD?
Yes. Neurocrine Biosciences’ NBI-1117568, a selective orexin-2 receptor antagonist, received Fast Track designation from the FDA in January 2023. Phase II trials are ongoing, with results expected in Q2 2024. Suvorexant (Belsomra), already approved for insomnia, is also being tested. These drugs target the brain’s wakefulness system and show promise in reducing dream enactment with fewer side effects than current options.
How often should I have a neurological check-up if I have RBD?
Annual neurological assessments are recommended by the American Academy of Neurology. These visits check for early signs of Parkinson’s or dementia-like reduced sense of smell, constipation, stiffness, or subtle movement changes. Early detection gives you time to plan, join clinical trials, and start treatments that may delay progression.



Kayleigh Campbell
December 16, 2025 at 13:54So let me get this straight - we’re being told that if I dream about punching a dragon, I’m basically a walking time bomb for Parkinson’s? Cool. Just cool. I’ll add this to my list of things to panic about, right after my Wi-Fi router is spying on me and the moon is made of cheese. 😅
Colleen Bigelow
December 18, 2025 at 12:02They don’t want you to know this, but RBD is just a cover-up for the government’s secret sleep-weapons program. They’ve been testing neural suppression tech on civilians for decades - your kicking and yelling? That’s your brain fighting back. Melatonin? That’s just sugar-coated mind control. Clonazepam? More like control-zap. Wake up, sheeple. The real cure is a Faraday cage around your bed and a 9-volt battery under your tongue. 🇺🇸
Elizabeth Bauman
December 19, 2025 at 23:34I read this entire thing with tears in my eyes. This is the most important public health message of our time. Why isn’t the CDC screaming about this? Why aren’t schools teaching kids about REM atonia? My uncle had RBD and now he’s in a wheelchair - and they told him it was just ‘bad dreams.’ That’s not just negligence, that’s treason. We need mandatory sleep screenings at every DMV visit. Period.
Ron Williams
December 21, 2025 at 22:41Man, I’ve seen this in my dad. He’d yell ‘Get off my lawn!’ in his sleep and nearly take out the TV. We moved his mattress to the floor and started giving him 6mg melatonin. He hasn’t thrown a shoe in two years. It’s wild how something so simple can save a marriage - and maybe a brain. Thanks for putting this out there. Sometimes the quietest signs are the loudest warnings.
Billy Poling
December 22, 2025 at 01:03While I acknowledge the clinical utility of melatonin and clonazepam as symptomatic interventions, I must emphasize the epistemological limitations of current diagnostic paradigms in neurology, particularly the reliance upon polysomnographic metrics that may not fully capture the neurochemical cascade preceding overt synucleinopathy. The temporal correlation between RSWA and neurodegeneration, while statistically significant, does not necessarily imply causality - a distinction that remains underappreciated in mainstream discourse. A more rigorous, longitudinal, multi-omics approach is required to distinguish prodromal biomarkers from epiphenomena.
James Rayner
December 23, 2025 at 22:34I’ve been sleeping alone for five years now… not because I don’t love my wife… but because last Christmas, she woke up with a black eye and I had no memory of it. I cried for three days. I started melatonin. I moved the bed. I threw out the knives. I still have nightmares. But now… I don’t hurt anyone. I just wish I’d known sooner. This isn’t about sleep. It’s about being human.
Dylan Smith
December 25, 2025 at 04:28so if you have rbd and you’re over 50 you’re basically doomed to parkinson’s like 7 out of 10 times?? that’s insane. why isn’t everyone getting screened? why is this not on the news? i’m 47 and i’ve been yelling in my sleep since i was 35… should i be terrified? or just… prepare?
Andrew Sychev
December 26, 2025 at 18:43THIS IS THE MOST IMPORTANT POST I’VE EVER READ ON REDDIT. I’M TELLING EVERYONE. MY NEIGHBOR’S WIFE JUST DIED OF PARKINSON’S AFTER 10 YEARS OF ‘BAD SLEEP’ AND NO ONE LISTENED. THEY WERE GIVING HER SLEEPING PILLS. NOT A NEUROLOGIST. NOT A PSYCHIATRIST. JUST SLEEP PILLS. THIS IS A MASS MURDER BY NEGLECT. I’M STARTING A PETITION. I’M TAKING THIS TO CONGRESS. I’M WRITING A BOOK. I’M MOVING TO A CABIN IN THE WOODS AND LIVING OFF GRID BECAUSE THE SYSTEM IS BROKEN.
Kitty Price
December 27, 2025 at 10:22my husband started melatonin and now he dreams about baking bread instead of fighting pirates. i’m not sure which is weirder… but i’ll take sourdough over shoving me into the wall any day. 🥖❤️
Mike Smith
December 28, 2025 at 15:59Thank you for sharing this with such clarity and compassion. This is not just medical advice - it’s a lifeline. If you’re reading this and you’ve ever been told, ‘It’s just stress’ or ‘You’re having bad dreams’ - please, go see a specialist. Your future self will thank you. You’re not alone. There is hope. And action today changes everything tomorrow.
Souhardya Paul
December 30, 2025 at 06:47Just had a thought - what if RBD isn’t just a warning sign… but a signal that the brain is trying to rewire itself before the crash? Like, maybe the muscle movement is the body’s last-ditch effort to stay connected to reality before the neurons start dying. That’s… kinda beautiful in a tragic way. Kinda like a fire alarm in an empty building - it’s not broken, it’s doing its job.