Taking five or more prescriptions at once isn’t unusual-it’s becoming the norm. Nearly 41% of adults over 75 are managing that many medications daily. And while each one treats a real condition-high blood pressure, diabetes, arthritis, depression-the real danger isn’t the number of pills. It’s what happens when they interact. A single wrong combination can send you to the ER, cause kidney failure, or even lead to a fatal bleed. The good news? You don’t have to guess. Coordinating your prescriptions isn’t complicated. It just needs a system.
Keep a Complete, Updated Medication List
Start with what’s in your medicine cabinet. Not just prescriptions. Include every over-the-counter pill, vitamin, herb, and supplement. Many people forget these, but they’re often the source of hidden problems. For example, taking ibuprofen with blood thinners can cause stomach bleeding. St. John’s Wort can make antidepressants useless or dangerous. Your list needs details: brand name, generic name, dosage (like "Lisinopril 10mg"), how often ("once daily"), when ("with breakfast"), and why ("for high blood pressure"). Write it down. Or better yet, use your phone’s notes app. Update it every time your doctor adds, removes, or changes a dose. Bring this list to every appointment-even if you think you’ve told them before. Pharmacists see hundreds of patients a day. They won’t remember your history unless you give them the full picture.Use One Pharmacy for Everything
Splitting prescriptions between three different pharmacies is a recipe for disaster. Each pharmacy only sees part of your用药 history. That means they can’t catch interactions. A 2023 study in Health Affairs found that patients using a single pharmacy had 47% fewer dangerous drug interactions than those who shopped around. Your pharmacist is your best ally. They’re trained to spot conflicts between medications-even ones your doctor didn’t know about. When you fill all your prescriptions at one place, they build a complete profile. They can flag risks like combining a statin with grapefruit juice, or mixing a sleep aid with an antihistamine that causes dizziness. And if you’re on Medicare Part D, you’re eligible for free Medication Therapy Management (MTM) sessions. Pharmacists spend 20-25 minutes reviewing your entire list. No charge. No appointment needed in many cases.Try Medication Synchronization
Imagine getting all your monthly prescriptions ready on the same day. No more juggling refill dates. No more running out of one pill while another is still in stock. That’s medication synchronization-a program offered by most community pharmacies. Here’s how it works: You pick one day each month-say, the first Tuesday. The pharmacy aligns all your maintenance meds (the ones you take daily) to refill on that day. If you’re due for a refill on the 5th, they’ll give you a partial supply now so it lines up with the 1st. You pick everything up at once. It cuts down on missed doses by 31%, according to the American Society of Health-System Pharmacists. It also means your pharmacist checks your entire regimen every month. They’ll ask: "Are you still taking this?" "Is this side effect getting worse?" "Can we lower this dose?" This kind of regular review reduces hospital visits by 22% and cuts emergency room trips by nearly 18%.
Use a Pill Organizer-But Make It Work for You
A simple plastic box with seven compartments-AM and PM-is one of the cheapest, most effective tools you can use. But only if you use it right. Fill it once a week. Sunday night works best for most people. Make it part of a routine: while you watch your favorite show, pour your pills into the slots. Label them if you need to. Some organizers come with alarms, like the Hero Health device, which costs around $900. It’s expensive, but studies show it improves adherence by 39% compared to basic boxes. If you can’t afford a smart device, a basic one still helps. A 2023 study in the Journal of General Internal Medicine tracked 1,245 older adults. Those using a 7-day organizer saw their adherence jump from 62% to 87% in just six months. That’s not magic. That’s structure.Watch Out for These Common Dangerous Combinations
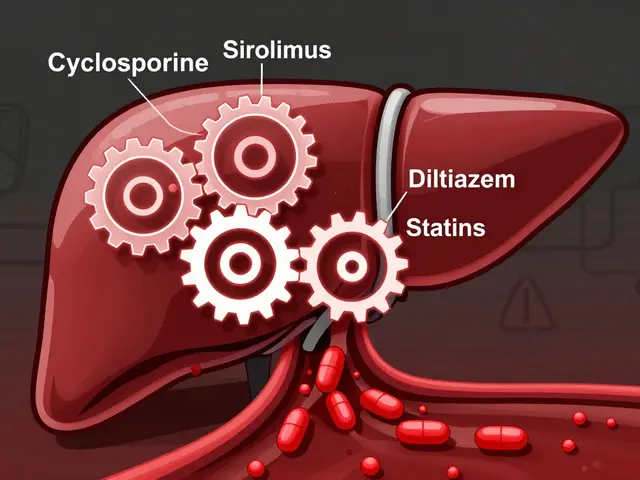
Some interactions are so common, they’re almost predictable. The American Geriatrics Society’s 2023 Beers Criteria lists 30 risky combos to avoid. Here are three you need to know:- NSAIDs (like ibuprofen) + blood pressure meds: These can cause kidney damage and make your BP harder to control.
- Calcium supplements + thyroid medication: Take them at least two hours apart. Calcium blocks absorption-your thyroid pill won’t work.
- Proton pump inhibitors (like omeprazole) + clopidogrel: The acid reducer can cancel out the blood thinner’s effect, raising stroke risk.
Know When to Ask About Deprescribing
Not every pill you’ve taken for years still needs to be there. Sometimes, the risks outweigh the benefits. That’s where deprescribing comes in. It’s not quitting meds cold turkey. It’s a slow, careful process-done with your doctor-to reduce or stop drugs that no longer help. For example, if you’re 80 and take a statin for high cholesterol but have no history of heart disease, your doctor might consider lowering the dose or stopping it. If you’re on three sleeping pills and still wake up tired, maybe one can go. The goal isn’t to cut pills for the sake of it. It’s to improve how you feel. The American Geriatrics Society, the American Society of Health-System Pharmacists, and the American Psychiatric Association all agree: regularly review your meds. Ask: "Is this still helping?" "Could it be causing more harm?" Many patients feel guilty asking. But your doctor wants you to ask. They can’t read your mind. If you’re dizzy, confused, or nauseous more than usual, it might not be aging. It might be your meds.
Use Digital Tools Wisely
Apps like Medisafe and MyMeds send reminders, track refills, and log side effects. In a 2022 JAMA study, users had 28% higher adherence than those using paper logs. But here’s the catch: 62% of adults over 75 don’t use smartphones regularly. If you’re not comfortable with apps, don’t force it. A paper list and a pill box work just fine. If you do use an app, pick one that lets you share your list with family or your pharmacist. CVS’s app, for example, sends a 72-hour refill alert. That cut missed doses by 28% in a trial of over 3,000 patients. The key is consistency-not fancy features.What to Do If You Notice New Side Effects
Drowsiness. Confusion. Upset stomach. Dizziness. These aren’t just "getting older." They’re red flags. Eighty-two percent of dangerous interactions happen because patients don’t tell their doctors about new symptoms-or they don’t mention the supplements they’re taking. If you feel different after starting a new med or changing a dose, write it down. Note the date, the symptom, and when it happens. Bring it to your next visit. Don’t wait. A simple change-like switching from a long-acting painkiller to a shorter one-can eliminate side effects without losing pain control.Final Checklist: Your Action Plan
- Make a full list of every pill, vitamin, and supplement-including doses and times.
- Fill all prescriptions at one pharmacy.
- Ask if your pharmacy offers medication synchronization.
- Use a 7-day pill organizer. Fill it every Sunday.
- Review your list with your pharmacist every 3 months.
- Ask your doctor: "Is there a medication I can stop?"
- Never start a new supplement without checking with your pharmacist first.
Coordinating prescriptions isn’t about being perfect. It’s about being consistent. One small step-like using one pharmacy or filling a pill box weekly-can prevent a hospital trip. And in a system where medication errors cause over 277,000 deaths a year in the U.S., those small steps aren’t just helpful. They’re life-saving.
What should I do if I’m taking more than five medications?
Start by making a complete list of all your medications, including over-the-counter drugs and supplements. Take that list to your pharmacist and ask for a medication review. Ask if your pharmacy offers medication synchronization to simplify refills. Then, schedule a deprescribing conversation with your doctor-ask if any medications can be reduced or stopped safely.
Can I just stop a medication if I think it’s causing side effects?
No. Stopping some medications suddenly can be dangerous-for example, blood pressure or antidepressant pills. Instead, write down your symptoms and when they started. Bring them to your doctor or pharmacist. They can help you safely adjust your dose or switch to a different drug.
Why does my pharmacist ask about supplements?
Because many supplements interact with prescription drugs. For example, garlic, ginkgo, and fish oil can thin your blood and increase bleeding risk if you’re on warfarin. St. John’s Wort can make antidepressants or birth control pills ineffective. Pharmacists are trained to spot these hidden risks-so always tell them everything you’re taking.
Is medication synchronization free?
Yes, in most cases. Most community pharmacies offer medication synchronization at no extra cost. It’s part of their service to improve adherence and reduce hospitalizations. Medicare Part D beneficiaries are also eligible for free Medication Therapy Management sessions, which include synchronization and full regimen reviews.
How do I know if a pill organizer is right for me?
If you miss doses, forget if you’ve taken your pills, or take them at the wrong time, a pill organizer can help. Even a basic one with AM/PM compartments improves adherence by over 25%. If you’re comfortable with technology, consider a smart organizer with alarms. If not, a simple plastic box works just as well-just make sure you fill it consistently, like every Sunday night.




Mandy Kowitz
January 4, 2026 at 06:44So let me get this straight-we’re supposed to trust a pharmacist who can’t even remember my name but somehow knows my entire medication history better than my own doctor? Sure. Next they’ll tell me my tea is causing my heart to skip beats.
Dee Humprey
January 5, 2026 at 18:12This is actually one of the most practical guides I’ve seen on med management. Seriously. I’ve been helping my mom with her pills for years-this checklist? Gold. 🙌
Vicki Yuan
January 7, 2026 at 13:55Using a single pharmacy isn’t just smart-it’s statistically proven to reduce adverse events by nearly half. The data is clear, and yet so many patients still hop between CVS, Walgreens, and that sketchy corner store that sells vitamins next to the lottery tickets. It’s not laziness. It’s negligence.
en Max
January 9, 2026 at 07:30Medication synchronization, as defined by the American Society of Health-System Pharmacists (ASHP), is a structured, evidence-based intervention that aligns refill cycles to optimize adherence, reduce polypharmacy-related errors, and facilitate proactive clinical review. It is not merely a logistical convenience-it is a clinical quality metric.
Enrique González
January 9, 2026 at 11:18I’ve been taking seven meds for 8 years. I use a pill box, one pharmacy, and I write everything down. It’s not hard. It’s just discipline. And yeah-I still forget sometimes. But now I don’t end up in the ER.
Aaron Mercado
January 11, 2026 at 04:08Wait… so if I take St. John’s Wort with my antidepressant… I’m basically doing a slow-motion suicide?!!?? I thought it was just a "natural mood booster"… I’m calling my pharmacist RIGHT NOW.
bob bob
January 11, 2026 at 05:19My grandma started using a 7-day organizer and now she’s laughing again. She used to be so tired all the time-turns out two of her meds were making her zombified. She didn’t even realize it was the pills. Just thought she was "getting old."
Angie Rehe
January 11, 2026 at 11:20Why are we letting pharmacists be the gatekeepers of our medication safety? This is a systemic failure of the medical-industrial complex. Doctors are overworked, pharmacists are underpaid, and patients are left to play Jenga with their own lives. You want change? Demand better coordination-not another pill box.
Jason Stafford
January 11, 2026 at 15:26They didn’t mention the real issue: Big Pharma is designing drugs to interact. That’s why they patent combinations. Why else would they push you to take five pills instead of one? They make more money when you’re sick. This whole system is rigged.
And don’t get me started on "natural supplements"-they’re all secretly laced with active ingredients the FDA doesn’t regulate. Your fish oil? Probably contains a banned stimulant. Your turmeric? Mixed with corticosteroids. You think you’re being healthy? You’re being experimented on.
My cousin’s neighbor’s cousin died after taking garlic pills with blood thinners. They found traces of warfarin in the supplement bottle. No one was charged. Why? Because the FDA is owned by the same people who own the pharmacies.
They want you to trust the system. Don’t. Write everything down? Fine. Use one pharmacy? Okay. But never assume it’s safe. Always question. Always verify. Always look up the batch number. Always.
I’ve seen the documents. They’re not mistakes. They’re features.
Justin Lowans
January 13, 2026 at 02:16It’s heartening to see such a comprehensive, clinically grounded approach to polypharmacy management. The emphasis on medication reconciliation, pharmacist engagement, and deprescribing aligns precisely with current geriatric best practices as outlined by the Beers Criteria and the American Geriatrics Society. The data cited-particularly the 47% reduction in interactions via single-pharmacy use-is not merely anecdotal but corroborated by peer-reviewed epidemiological studies. This is precisely the kind of patient-centered, systems-based thinking that must be scaled across primary care networks.
That said, I would encourage further integration of electronic health record interoperability to automate medication list updates. A patient’s list should update in real time when a new prescription is issued, reducing reliance on manual entry. Additionally, the use of AI-driven clinical decision support tools could flag high-risk combinations before the prescription is even filled. These are not luxuries-they are necessities in an aging population.
Thank you for elevating this conversation beyond mere compliance to one of dignity, safety, and autonomy.
saurabh singh
January 13, 2026 at 14:20Bro, in India, we don’t have pharmacies like this. My dad takes 8 pills and he just puts them in a tin box with sticky notes. But he knows what each one does because he’s been doing it for 15 years. You don’t need fancy apps-you need someone who cares. My aunt? She checks his pills every Sunday. That’s the real system.
Also, St. John’s Wort? Yeah, we call it "hypericum" and everyone knows it kills antidepressants. But here’s the thing: if your family doesn’t ask you about your meds, no pharmacist will. Talk to your people. That’s the real magic.
Michael Rudge
January 13, 2026 at 17:38Oh, so now we’re supposed to believe that a $900 smart pill organizer is the pinnacle of medical innovation? Meanwhile, people are dying because their doctor didn’t bother to ask if they were taking ginkgo. This isn’t a tech problem. It’s a moral failure. You’re treating symptoms with gadgets while ignoring the root cause: doctors who don’t listen, and a system that profits from confusion.
And let’s be honest-if your medication list is so complicated that you need an app to remember it, maybe you shouldn’t be taking all those pills in the first place.
Dee Humprey
January 14, 2026 at 23:16Just got my mom’s new pill box filled for the week. She’s been using this system for 6 months. No more double-dosing. No more "I thought I already took that." She says she feels like she has her life back. 💙