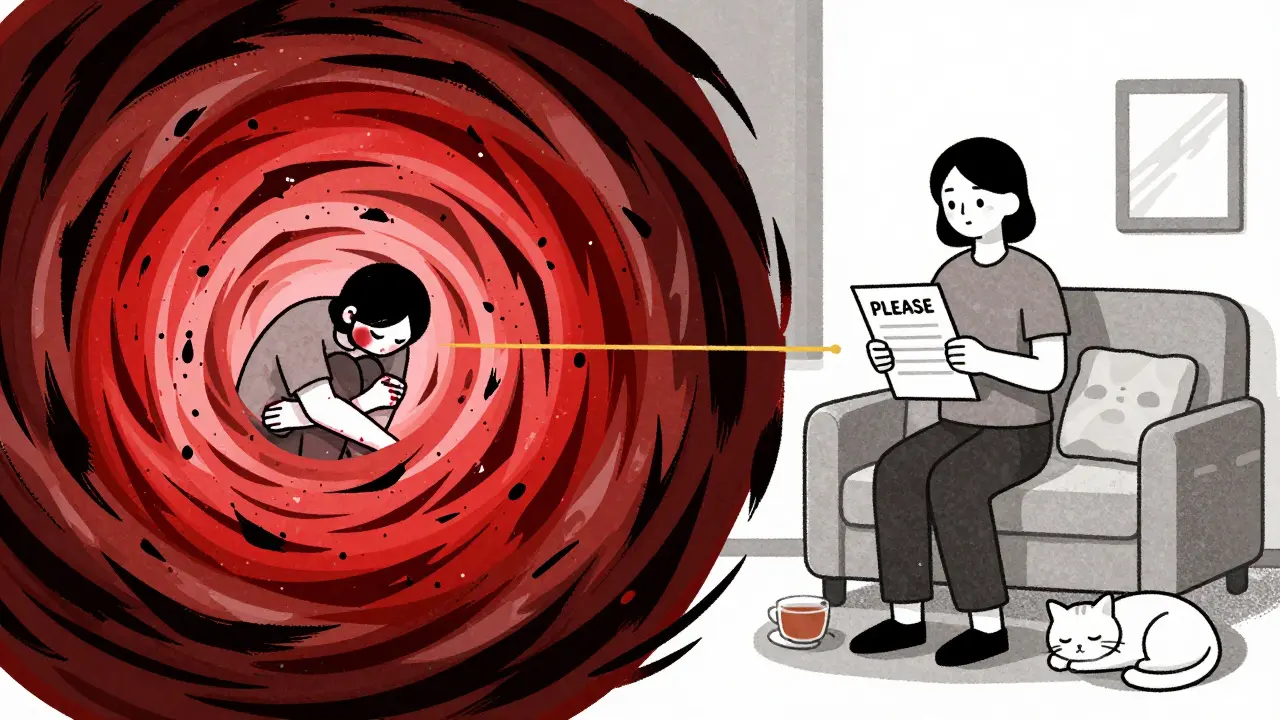
When you’re living with borderline personality disorder (BPD), emotions don’t just come and go-they crash over you like a wave with no shore. One moment you’re fine, the next you’re overwhelmed, desperate, or convinced you’re unlovable. Self-harm, impulsive decisions, and relationship meltdowns aren’t choices-they’re survival responses to pain no one else seems to understand. That’s where DBT skills come in. Not as a cure, but as a lifeline.
What DBT Actually Does for BPD
Dialectical Behavior Therapy, or DBT, wasn’t created to make people feel better in theory. It was built by Dr. Marsha Linehan in the late 1980s because standard therapy kept failing people with BPD who were in constant crisis. These weren’t people being dramatic-they were drowning in emotions they couldn’t control, and no one had given them tools to swim. DBT works because it’s practical. It doesn’t just talk about feelings; it teaches you how to handle them. The therapy combines two opposing ideas: accepting yourself as you are right now, and changing behaviors that hurt you. That’s the “dialectical” part-holding both truths at once. You’re not broken. But you can learn to stop hurting yourself. Research shows DBT cuts self-harm by nearly half compared to regular therapy. In one major study, suicide attempts dropped by 50% after a year of DBT. That’s not a small win. That’s life-changing.The Four Core Skill Modules
DBT isn’t one thing. It’s four skill sets, each designed to tackle a different part of the BPD storm.Mindfulness: Grounding Yourself in the Now
Mindfulness in DBT isn’t about sitting quietly and breathing. It’s about learning to notice what’s happening inside you without panicking. The goal? To step out of automatic reactions and into awareness. You learn three “what” skills: observe (notice your thoughts and feelings), describe (put words to them), and participate (jump into the moment without overthinking). And three “how” skills: do it non-judgmentally, one-mindfully (focus on one thing at a time), and effectively (get what you need without making things worse). A study found that after just eight weeks of mindfulness practice, people with BPD improved their emotional regulation by 32%. That means you start noticing anger or panic earlier-and you have a chance to respond before it explodes.Distress Tolerance: Getting Through the Impossible Moments
This is where DBT shines. When you’re in crisis-when the pain is too much, and you feel like you can’t take another second-what do you do? DBT gives you concrete tools to survive without self-harm:- TIPP: Change your body to calm your mind. Splash ice water on your face. Do 20 jumping jacks. Breathe slowly for 30 seconds. Tighten and release your muscles. These physical tricks interrupt the panic cycle.
- ACCEPTS: Distract yourself with activities you can control: watch a funny video, call a friend, clean your room, play a game. Don’t wait for the feeling to pass-change your focus.
- IMPROVE: Use imagery (picture yourself safe), find meaning in the pain, pray or meditate, relax your body, focus on one thing in the moment, take a mental vacation, or give yourself encouragement.
Emotion Regulation: Understanding and Changing Your Emotional Engine
You don’t have to be ruled by your emotions. DBT teaches you how to read them, reduce their intensity, and respond to them wisely.- PLEASE: Treat physical illness, eat balanced meals, avoid drugs and alcohol, sleep enough, and move your body. These aren’t “nice-to-haves.” They’re survival basics. Your brain can’t regulate emotion if you’re exhausted, hungry, or high.
- ABC: Accumulate positive emotions (do things you enjoy), build mastery (do things you’re good at), and cope ahead (plan for hard situations before they happen).
- Opposite Action: If you feel like isolating because you’re ashamed, reach out. If you want to lash out in anger, speak gently. Do the opposite of your urge.
Interpersonal Effectiveness: Holding Your Ground Without Losing Yourself
Relationships are the biggest trigger for people with BPD. Fear of abandonment leads to clinging, rage, or pushing people away. DBT gives you scripts to speak up without destroying connections.- DEAR MAN: Describe the situation. Express your feelings. Assert your need. Reinforce the positive outcome. Stay mindful. Appear confident. Negotiate if needed.
- GIVE: Be gentle. Show interest. Validate the other person. Use an easy manner. This keeps people from feeling attacked.
- FAST: Be fair to yourself and others. No unnecessary apologies. Stick to your values. Be truthful.
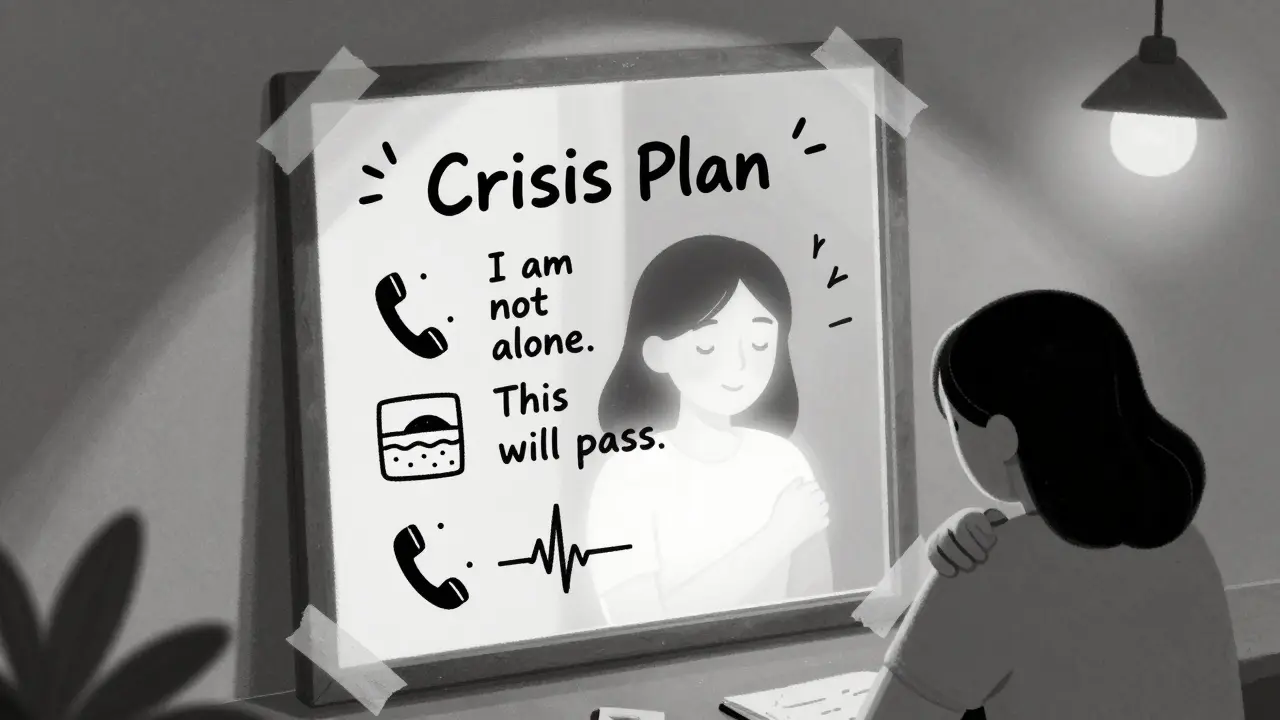
Crisis Planning: Your Personal Emergency Kit
A crisis plan isn’t a vague “I’ll call someone.” It’s a written, step-by-step guide for when your brain shuts down. Here’s how to build one:- Identify your top three warning signs: What do you feel, think, or do before a crisis? (e.g., “I can’t breathe,” “I feel like I’m disappearing,” “I start cutting.”)
- List your go-to DBT skills: TIPP? IMPROVE? STOP? Pick the ones that work for you.
- Write down your support network: Who can you call? Who won’t panic? Keep names and numbers in your phone and on paper.
- Include distractions: A playlist, a movie, a puzzle book, a pet to cuddle.
- Add a safety statement: “I am not alone. This feeling will pass. I have survived this before.”
- Store it where you can find it: On your phone, taped to your mirror, in your wallet.
How DBT Compares to Other Treatments
There are other therapies for BPD. But DBT stands out.- Mentalization-Based Therapy (MBT) focuses on understanding your own and others’ mental states. It helps with identity issues but doesn’t give you crisis tools.
- Schema Therapy digs into deep childhood patterns. It’s powerful, but slow.
- STEPPS is a group program that teaches DBT skills in 20 weeks. It helps with symptoms but doesn’t replace individual therapy or crisis coaching.
What It Really Takes to Make DBT Work
You don’t need to be perfect. You just need to be willing to try. Most people take 2-4 weeks to understand the basics. Mastery? That takes 6-8 months. The first month is rough. You’ll feel overwhelmed. You’ll forget your skills. You’ll think, “This isn’t working.” But here’s what happens if you stick with it:- By month 3, you start noticing triggers before they hit.
- By month 6, you’re using skills without thinking.
- By month 12, you’re surprised by how calm you feel during fights, breakups, or rejections.
What People Really Say About DBT
On Reddit’s r/DBT community, people share raw, honest stories:- “I keep the PLEASE checklist on my fridge. When I feel like I’m falling apart, I check: Did I eat? Sleep? Move? If not, I fix that first.”
- “My therapist never said I was too sensitive. She said, ‘Your feelings are real. Now let’s find a way to survive them.’ That changed everything.”
- “I used GIVE with my mom during a huge fight. I didn’t yell. I didn’t leave. I said, ‘I love you, and I’m scared.’ She cried. We hugged.”
Where to Start
If you think DBT could help you:- Find a therapist certified in DBT. Look at the Linehan Institute’s directory or ask your doctor.
- Ask if they offer a full program: individual therapy, skills group, phone coaching, and therapist consultation team.
- Get the workbook: The Dialectical Behavior Therapy Skills Workbook is a solid starting point.
- Print out the TIPP, STOP, and PLEASE sheets. Tape them where you’ll see them.
- Start small. Pick one skill. Use it once a day. Even if it feels silly.
Is DBT Right for You?
DBT works best if you struggle with:- Intense emotions that feel uncontrollable
- Self-harm or suicidal thoughts
- Chaotic relationships
- Feeling empty or disconnected
- Impulsive actions you regret later
Final Thought: You’re Not Broken
BPD isn’t a personality flaw. It’s a survival system that got stuck. You learned to cope with pain the only way you knew how. DBT doesn’t erase that. It gives you new tools so you don’t have to keep hurting yourself to survive. You don’t need to be “fixed.” You just need to learn how to hold yourself gently while you heal.Can DBT help with suicidal thoughts?
Yes. DBT is one of the most effective treatments for reducing suicidal behavior in people with BPD. Research shows it cuts suicide attempts by 50% over the first year. Skills like TIPP, STOP, and IMPROVE are designed specifically to help you survive moments of crisis without acting on suicidal urges. Phone coaching gives you real-time support when you feel you can’t go on.
How long does DBT take to work?
You’ll start noticing small changes within 2-4 weeks-like recognizing your triggers earlier or pausing before reacting. But real skill mastery takes 6-8 months of consistent practice. Most full DBT programs last 6 to 12 months. The goal isn’t to “get better” quickly-it’s to build habits that last a lifetime.
Do I need to do group therapy for DBT?
Full DBT includes both individual therapy and skills group training. The group teaches you the skills, gives you practice with peers, and reduces shame by showing you’re not alone. But if group isn’t available, individual therapy with a trained DBT therapist can still help. Some apps and workbooks also offer structured skill training if groups aren’t accessible.
Can I do DBT on my own without a therapist?
You can learn the skills from books and apps, and many people do. But DBT was designed as a full system: individual therapy, group, phone coaching, and therapist consultation. Doing it alone increases the risk of misunderstanding the skills or giving up during hard moments. A therapist helps you apply them correctly and stay accountable. If you can’t find a therapist, start with the workbook and reach out to online communities like r/DBT for support.
Is DBT covered by insurance?
Yes, in most cases. Medicare and private insurers in the U.S. typically cover 12-20 DBT sessions per year for BPD. The program must follow the standard Linehan Model (individual therapy, group, phone coaching) to qualify. Ask your provider if they accept insurance for DBT. Telehealth options have made access easier, especially in rural areas.
What if I can’t find a DBT therapist near me?
Telehealth has expanded access dramatically since 2020. Many certified DBT therapists now offer virtual sessions. Check the Linehan Institute’s directory or search for “online DBT therapy.” Apps like DBT Coach and Virtual Reality DBT can supplement your learning. You can also join peer support groups on Reddit or Facebook. You’re not alone-and help is more available than ever.
Can DBT help with anger and rage?
Absolutely. Anger is one of the most common and overwhelming emotions in BPD. DBT’s emotion regulation skills-especially opposite action and PLEASE-are built for this. Instead of exploding, you learn to recognize anger early, reduce its intensity with physical techniques (like TIPP), and respond with assertiveness (DEAR MAN) instead of aggression. People report feeling less out of control after just a few months of practice.
Are DBT skills useful for people without BPD?
Yes. Many people without BPD use DBT skills to manage anxiety, depression, trauma, or just everyday stress. Mindfulness, distress tolerance, and emotional regulation are universal tools. You don’t need a diagnosis to benefit from learning how to pause, breathe, and respond instead of react.



Sarah Williams
December 20, 2025 at 23:29Just wanted to say this post saved my life. I’ve been using TIPP every time I feel like I’m going to break. Ice water on my face? Yeah, it’s weird. But it works. I’ve gone from 3 self-harm episodes a week to zero in two months. DBT isn’t magic-it’s muscle. And I’m finally building it.
Peggy Adams
December 21, 2025 at 03:33Yeah right. Like the government isn’t pushing this so we stop screaming about how broken the system is. DBT? More like Distract-Breathe-Trust-the-system. They don’t want us to fix the world-they want us to fix ourselves so we stop demanding change.
Theo Newbold
December 21, 2025 at 04:20The data is cherry-picked. 50% reduction in suicide attempts? Compared to what? Wait-list controls? That’s not a robust comparison. And where’s the long-term follow-up? Most studies show effects plateau after 18 months. Also, the sample sizes are tiny. This isn’t evidence-it’s advocacy.
Erika Putri Aldana
December 21, 2025 at 16:41lol at all these ‘skills’. you think writing down ‘i am not alone’ on a sticky note fixes trauma? you’re just being taught to suck it up so the system doesn’t have to pay for real care. they want you to meditate while your rent goes up and your meds get denied. this isn’t healing. it’s gaslighting with a worksheet.
Adrian Thompson
December 21, 2025 at 23:04DBT is just a corporate rebrand of obedience training. They took old behavioral techniques, slapped ‘dialectical’ on it, and sold it to hospitals as ‘cutting-edge.’ Meanwhile, the real problem? No one’s paying for housing, therapy, or food. But hey, here’s a 300-page workbook so you can learn to breathe while you starve.
Cameron Hoover
December 23, 2025 at 13:29I didn’t believe in this until I tried it. I used to scream at my sister every time she didn’t text back. Now? I use DEAR MAN. I said, ‘I feel scared when I don’t hear from you. I need to know you’re okay.’ She cried. We talked. I didn’t lose her. That’s not therapy-that’s magic. And I’m not even done yet.
Sandy Crux
December 23, 2025 at 22:26While the empirical support for DBT is statistically significant, one must interrogate the epistemological foundations of its operationalization-particularly the reductionist framing of affective dysregulation as a ‘skill deficit,’ thereby implicitly pathologizing normative human distress. The commodification of emotional labor under the guise of therapeutic innovation is, frankly, a neoliberal dystopia.
Hannah Taylor
December 24, 2025 at 13:35so i tried the stop skill and it made me feel worse?? like why am i supposed to just ‘observe’ when i feel like my skin is on fire?? this whole thing feels like being told to calm down while someone’s holding a lighter to your arm. also why is everyone on here acting like this is the only way?? what about meds?? what about trauma therapy??
Jason Silva
December 24, 2025 at 23:08bro i used IMPROVE last week during a panic attack and i literally imagined myself on a beach with a margarita 🌊🍹. i didn’t cut. i didn’t text my ex. i just… breathed. i’m not crying. you’re crying. this stuff works. trust the process. 🙏
mukesh matav
December 25, 2025 at 22:08Thank you for sharing this. I’m from India and DBT isn’t easily available here. But I read the workbook and practiced TIPP on my own. It’s not perfect, but it helped me stay alive. I don’t need a therapist to know that breathing through pain matters.
Jay lawch
December 26, 2025 at 16:45Let me break this down. DBT was created by a woman who was institutionalized herself. That’s not a coincidence. The entire framework is a psychological pacifier designed to keep the emotionally volatile from rising up against the system. The skills? They’re behavioral conditioning. The ‘crisis plan’? It’s a compliance checklist. The government funds this because it’s cheaper than fixing poverty, housing, or healthcare. You’re being trained to survive within a broken system-not to change it. The real trauma isn’t in your mind-it’s in the world they built.
Southern NH Pagan Pride
December 27, 2025 at 06:57DBT is not therapy. It is a cognitive restructuring protocol embedded within a neoliberal framework of self-management. The emphasis on individual behavioral modification obscures structural determinants of psychological distress. Furthermore, the certification model is proprietary and exclusionary, creating a gatekeeping apparatus that prioritizes institutional revenue over accessible care. The ‘skills’ are not tools-they are disciplinary techniques.