Eye Infection Symptom Checker
Eye Infection Assessment
Answer these questions to identify potential eye conditions. This tool is for informational purposes only and does not replace professional medical diagnosis.
When your eye turns red, it’s usually a warning that something’s gone wrong inside. Eye infection is a broad term for any microbial or inflammatory condition that makes the eye look blood‑shot, feel gritty, or swell up. Understanding which infection you’re dealing with is the first step toward relief.
What "red eye" actually means
Redness occurs when tiny blood vessels on the white part of the eye (the sclera) expand. The most common triggers are allergies, dry‑eye irritation, and, of course, infections. An infection adds a layer of danger because bacteria, viruses, or fungi can damage the cornea or spread to nearby structures if left untreated.
Typical culprits behind a red eye
Below is a quick rundown of the infections that most often turn your eye crimson.
- Conjunctivitis - inflammation of the thin membrane (conjunctiva) covering the eye and inner eyelid.
- Blepharitis - chronic inflammation of the eyelid margins.
- Keratitis - infection of the cornea, the clear front window of the eye.
- Stye (hordeolum) - a painful, pus‑filled lump on the eyelid edge.
- Uveitis - inflammation of the uveal tract (iris, ciliary body, choroid).
- Allergic conjunctivitis - reaction to pollen, pet dander, or cosmetics.
- Bacterial conjunctivitis - bacterial invasion of the conjunctiva.
- Viral conjunctivitis - usually caused by adenovirus.
- Dry eye syndrome - insufficient tear production that can mimic infection.
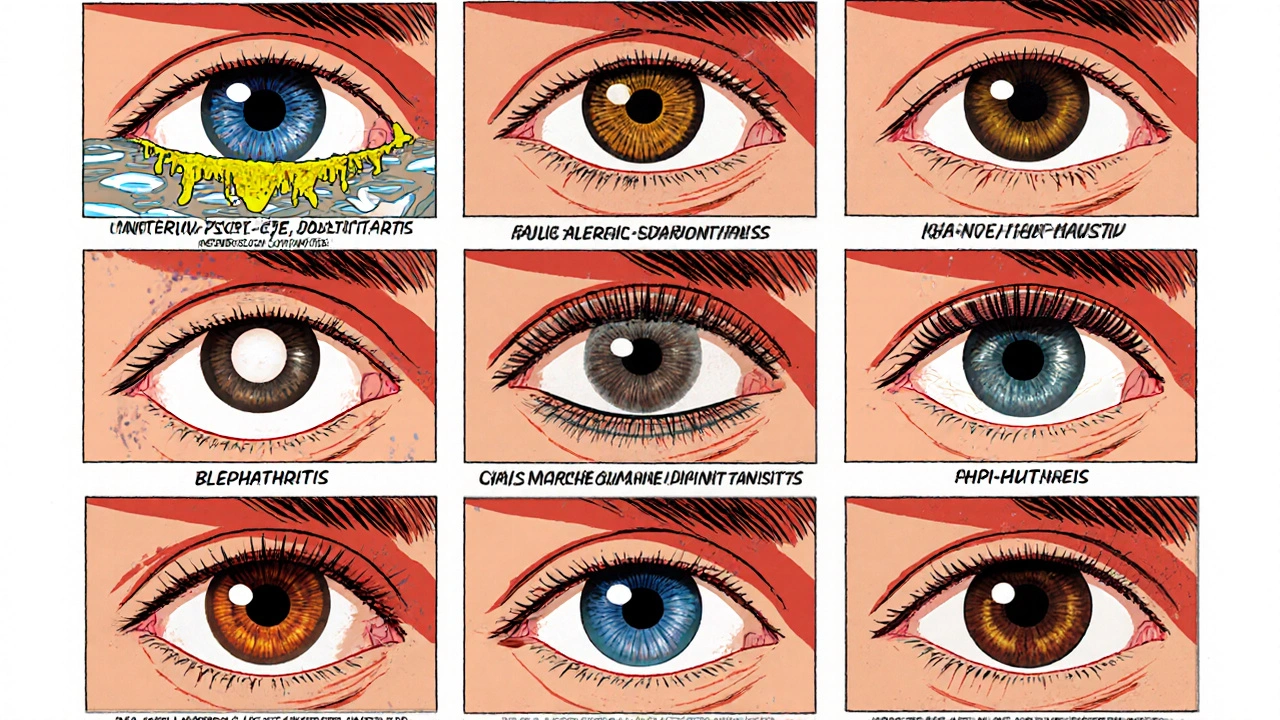
How to spot each infection
Knowing the hallmark signs helps you pick the right treatment.
Conjunctivitis (general)
Typical signs: sticky or watery discharge, itching, gritty feeling, and a uniformly red eye. The discharge may be clear (viral) or thick and yellow‑green (bacterial).
Blepharitis
Signs include crusty eyelid margins, burning, and flaking skin on the lashes. Redness often surrounds the lid rather than the whole eyeball.
Keratitis
Look for pain, blurred vision, extreme light sensitivity, and a white or gray spot on the cornea. A red eye with severe pain is a red flag for keratitis.
Stye (hordeolum)
A small, red bump at the edge of the lid that feels hot to the touch. It may develop a yellow tip as pus collects.
Uveitis
Sudden deep pain, colored rings (iris abnormalities), and blurred vision signal a more serious inflammation inside the eye. Redness is often accompanied by a pupil that looks smaller than the other.
Allergic conjunctivitis
Intense itching, watery discharge, and a stringy mucus are classic. Symptoms rise and fall with exposure to the allergen.
Bacterial conjunctivitis
Thick, sticky discharge that may crust over overnight, along with a gritty sensation and light redness. Usually starts in one eye and can spread to the other.
Viral conjunctivitis
Watery discharge, a burning sensation, and a pinkish hue that spreads quickly. Often accompanied by a cold or sore throat.
Dry eye syndrome
Burning, foreign‑body sensation, and intermittent redness that improves with blink breaks or artificial tears.
Treatment options for each infection
Below is a practical guide on what works best for each condition.
- Conjunctivitis
- Viral: Cool compresses, lubricating drops, and time-most clear up in 1‑2 weeks.
- Bacterial: Prescription antibiotic eye drops or ointments (e.g., azithromycin, ciprofloxacin) for 5‑7 days.
- Allergic: Antihistamine drops, oral antihistamines, and avoiding triggers.
- Blepharitis
- Warm compresses twice daily, lid‑scrub with diluted baby shampoo, and, if needed, topical antibiotics.
- Keratitis
- Urgent ophthalmology visit. Treatment may involve fortified antibiotic drops, antiviral medication (for herpes), or antifungal drops.
- Stye
- Warm compresses for 10‑15 minutes, 3-4 times a day. If it doesn't improve, a doctor may lance it or prescribe a topical antibiotic.
- Uveitis
- Systemic steroids or immunosuppressive drugs under specialist care. Immediate treatment prevents vision loss.
- Dry eye syndrome
- Artificial tears, punctal plugs, or prescription cyclosporine eye drops. Reduce screen time and use a humidifier.
Quick comparison of the most common red‑eye infections
| Feature | Viral | Bacterial | Allergic |
|---|---|---|---|
| Discharge | Watery, clear | Thick, yellow‑green | Stringy, watery |
| Itchiness | Mild | Low | High |
| Onset | Rapid, spreads fast | Gradual, often unilateral first | Seasonal or exposure‑linked |
| Treatment | Supportive care | Antibiotic drops/ointment | Antihistamine drops, avoid allergens |
When to seek professional help
Most mild infections improve with basic care, but you should see an eye doctor immediately if you notice:
- Severe pain or vision changes
- Sensitivity to light that won’t ease
- A white or gray spot on the cornea
- Persistent redness after 48 hours of home treatment
- Eye injury combined with redness
Delaying treatment for keratitis, uveitis, or advanced bacterial infections can lead to permanent vision loss.
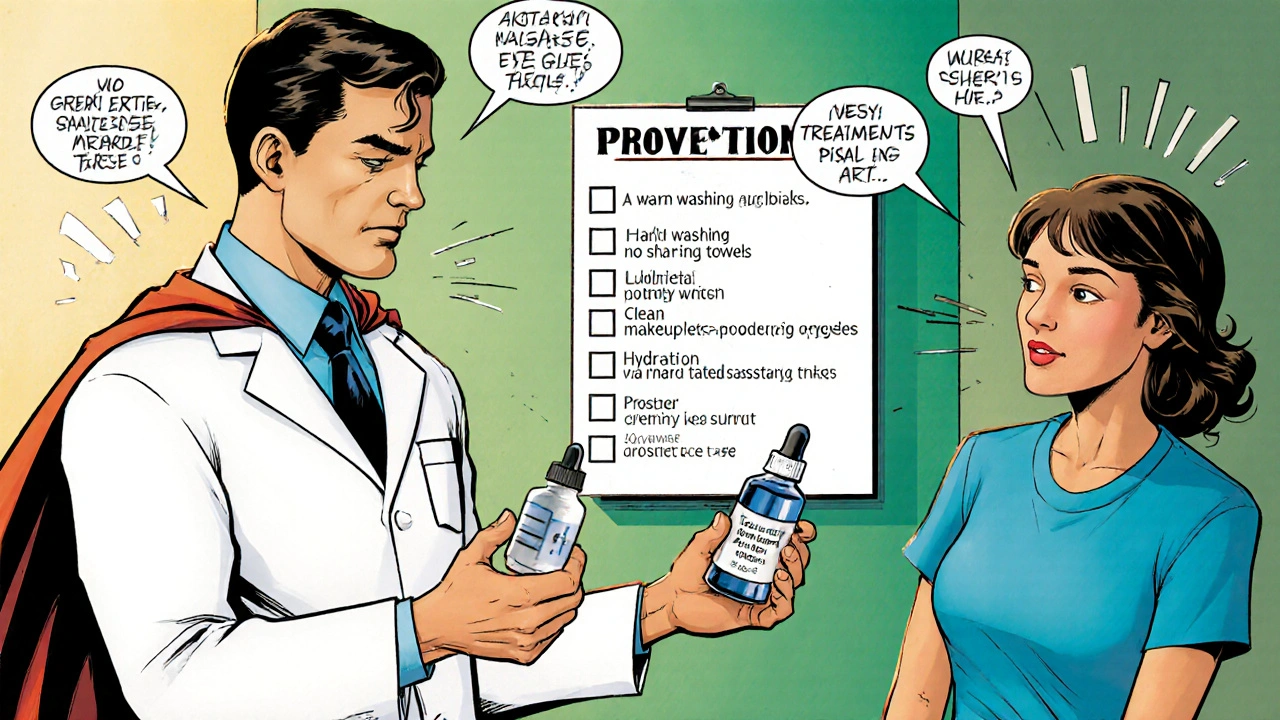
Prevention tips to keep your eyes clear
- Wash hands frequently, especially before touching your eyes.
- Avoid sharing towels, pillowcases, or makeup.
- Remove eye makeup before bed and replace old cosmetics every three months.
- Use protective eyewear when swimming or working with chemicals.
- Stay hydrated and blink often during screen time to reduce dry‑eye risk.
- Keep contact lenses clean; replace them on schedule.
By incorporating these habits, you’ll lower the odds of a painful red eye and catch any problem early.
Key takeaways
- Redness signals inflammation; infections are the most common cause.
- Identify the type-viral, bacterial, allergic, or other-by discharge, itchiness, and pain level.
- Mild cases often clear with warm compresses and lubricating drops; serious infections need prescription medication.
- Seek urgent care for pain, vision loss, or corneal spots.
- Simple hygiene habits dramatically cut down infection risk.
Frequently Asked Questions
Can I use over‑the‑counter eye drops for any red‑eye infection?
Artificial tears are safe for dryness and mild viral conjunctivitis, but they won’t treat bacterial infections. If discharge is thick or the eye hurts, see a doctor for targeted therapy.
How long does bacterial conjunctivitis stay contagious?
It’s usually contagious until 24‑48hours after starting antibiotic drops. Keep hands clean and avoid close contact during that window.
Is a stye an emergency?
Most styes respond to warm compresses and resolve in a week. If it grows rapidly, becomes very painful, or affects vision, get it checked - a doctor may need to drain it.
Why does my eye feel gritty when I have dry eye?
Tears lubricate the cornea; when the tear film is insufficient, the exposed surface irritates nerves, creating a sand‑like sensation. Artificial tears or prescription drops restore the moisture layer.
Can allergies cause a red eye that looks like an infection?
Yes. Allergic conjunctivitis produces watery, itchy eyes and a pink hue that mimics viral infection. The key difference is intense itching and a clear, stringy discharge rather than pus.

Alexis Howard
October 16, 2025 at 20:14Honestly the whole “warm compress” thing is overrated just blink more.
Darryl Gates
October 23, 2025 at 18:54Great rundown! For anyone dealing with a stye, remember that consistent warm compresses for 10‑15 minutes, three times a day, can speed up drainage and reduce pain.
Pair that with gentle lid hygiene-use a diluted baby‑shampoo solution and a clean cotton swab to wipe away crust.
If it doesn’t improve in a few days, a quick visit to your optometrist for a prescription ointment is the next logical step.
Kevin Adams
October 30, 2025 at 16:34Behold, the crimson tide that sweeps across the sclera, a drama of blood vessels and microbes!
One might ask, is the eye a battlefield or a theater? The answer lies in the secret choreography of tears and pathogens.
When viral adenovirus arrives, it paints the eye pink and whispers watery verses.
Bacterial invaders, on the other hand, scrawl thick, yellow‑green scripts upon the conjunctiva.
Allergic actors add relentless itching, a chorus of sneezes, and a flood of watery discharge-truly a tragicomedy of nature!
Katie Henry
November 6, 2025 at 15:14Esteemed readers, it is incumbent upon us to adopt vigilant ocular hygiene practices.
Regular hand washing, avoidance of shared cosmetics, and judicious use of protective eyewear constitute the pillars of prevention.
Should you encounter a red eye, initiate cool compresses and artificial tears without delay.
For manifestations of severe pain or visual disturbance, procure professional ophthalmic evaluation forthwith.
By adhering to these protocols, we safeguard our vision with the utmost diligence.
Joanna Mensch
November 13, 2025 at 13:54What the article fails to mention is the hidden agenda of the pharmaceutical conglomerates pushing over‑the‑counter drops as a universal cure.
They profit from our ignorance, ensuring we never question why a simple warm compress could be more effective than a pricey prescription.
Stay wary, keep your eyes clean, and don’t let the elite decide what you put in them.
RJ Samuel
November 20, 2025 at 12:34So you think a dab of eye drops solves everything? Think again.
Most over‑the‑counter solutions just mask symptoms while the underlying infection festers.
People need to realize that a proper diagnosis is the only way to target the right pathogen.
And yeah, washing your hands is still the single most effective preventive measure-no debate.
Patricia Echegaray
November 27, 2025 at 11:14Our nation’s liberty is being choked by a wave of imported eye‑care products that betray our health sovereignty.
These foreign ointments are laced with ingredients that keep us dependent on endless refills.
Only by returning to home‑grown, simple remedies-like warm compresses and saline rinses-can we reclaim control over our ocular wellbeing.
America first, even in eye health.
lisa howard
December 2, 2025 at 02:20Kevin, your theatrical description of red eye is certainly vivid, yet let us delve deeper into the practicalities of treatment.
First, the article glosses over the critical importance of differentiating discharge types; a clear, watery exudate typically signals viral involvement, whereas a purulent, yellow‑green secretion points toward bacterial etiology.
Second, while warm compresses are a cornerstone for styes, the temperature and duration matter; a soothing 40‑°C compress applied for ten to fifteen minutes, three times daily, optimizes liquefaction of the clogged meibomian glands.
Third, lid hygiene should not be dismissed as a mere afterthought-diluted baby‑shampoo or a commercially available lid‑scrub solution, applied with a clean cotton swab, reduces bacterial load and mitigates blepharitis.
Fourth, for suspected bacterial conjunctivitis, empiric therapy with a broad‑spectrum fluoroquinolone drops for five days can truncate the contagious period, but culture‑directed therapy is preferable when resistance is suspected.
Fifth, viral conjunctivitis, while self‑limiting, benefits from preservative‑free artificial tears to alleviate discomfort and prevent secondary bacterial superinfection.
Sixth, allergic conjunctivitis warrants antihistamine or mast‑cell stabilizer drops, and systemic antihistamines may provide additional relief when exposure to allergens is unavoidable.
Seventh, keratitis is a true ophthalmic emergency; any corneal opacity, severe photophobia, or visual acuity decline mandates immediate referral to an ophthalmologist for fortified antibiotic or antiviral therapy.
Eighth, uveitis, with its characteristic ciliary flush and miotic pupil, also demands prompt systemic corticosteroid therapy to avert irreversible damage.
Ninth, dry eye syndrome, often under‑diagnosed, can be managed with preservative‑free lubricants, punctal plugs, or prescription agents like cyclosporine A.
Tenth, lifestyle modifications-reducing screen time, employing humidifiers, and maintaining adequate hydration-are foundational preventive strategies.
Eleventh, the article omits the role of contact lens hygiene; improper lens care is a well‑documented risk factor for both microbial keratitis and conjunctivitis.
Twelfth, patient education on hand hygiene and avoiding eye rubbing cannot be overstated; these simple behaviors dramatically lower infection transmission.
Thirteenth, the tabular comparison is useful, yet clinicians should also consider patient age, immune status, and comorbidities when selecting therapy.
Fourteenth, follow‑up is essential; failure of symptoms to improve within 48‑72 hours should trigger re‑evaluation.
Finally, empowerment through knowledge enables patients to act swiftly, preserving sight and comfort.
In sum, a comprehensive, individualized approach-grounded in accurate diagnosis, appropriate pharmacotherapy, and diligent hygiene-remains the gold standard for managing red‑eye conditions.
Cindy Thomas
December 9, 2025 at 01:00Actually, the distinction between bacterial and viral conjunctivitis isn’t just about the color of the discharge; it also hinges on the duration and the presence of preauricular lymphadenopathy 😊.
Most people overlook that bacterial forms often resolve within 48‑72 hours of starting antibiotic drops, whereas viral cases linger up to two weeks.
Moreover, the article skipped over the fact that some viral strains can cause a secondary bacterial infection if left untreated.
So, while eye drops are handy, a proper assessment of symptoms over time is crucial.
James Falcone
December 15, 2025 at 23:40If you’re tired of global pharma pulling the strings, just stick to good old‑fashioned warm compresses and over‑the‑counter lubricants-no need for pricey imports.
Frank Diaz
December 22, 2025 at 22:20One must first acknowledge the epistemic humility required before prescribing any ocular medication.
Without a thorough differential diagnosis, the clinician risks perpetuating a cascade of iatrogenic complications.
Therefore, observation, patient history, and the judicious use of culture‑guided therapy should precede empiric treatment.
Mary Davies
December 29, 2025 at 21:00I’m curious why the guide didn’t highlight the role of contact lens hygiene in preventing keratitis, especially given how common lens‑related infections are today.
Valerie Vanderghote
January 5, 2026 at 19:40Reading through the list of infections makes me think we’re all just one sneeze away from a full‑blown eye crisis.
While the tips are solid, I’d add that moisturizing the air in your workspace can dramatically cut down on dry‑eye flare‑ups.
Also, never underestimate the power of a proper diet rich in omega‑3 fatty acids; they support tear film stability.
And if you wear makeup, replace it every six weeks-old mascara is a breeding ground for bacteria.
Finally, if you ever notice a persistent white spot on the cornea, don’t play hero; get to an eye specialist immediately.
Michael Dalrymple
January 12, 2026 at 18:20Your comprehensive overview serves as an excellent resource for both laypersons and clinicians.
By delineating each condition’s hallmark signs and corresponding therapeutic options, you empower readers to make informed decisions regarding when to self‑manage and when to seek professional care.
Keep up the diligent work; such clarity is invaluable in public health education.