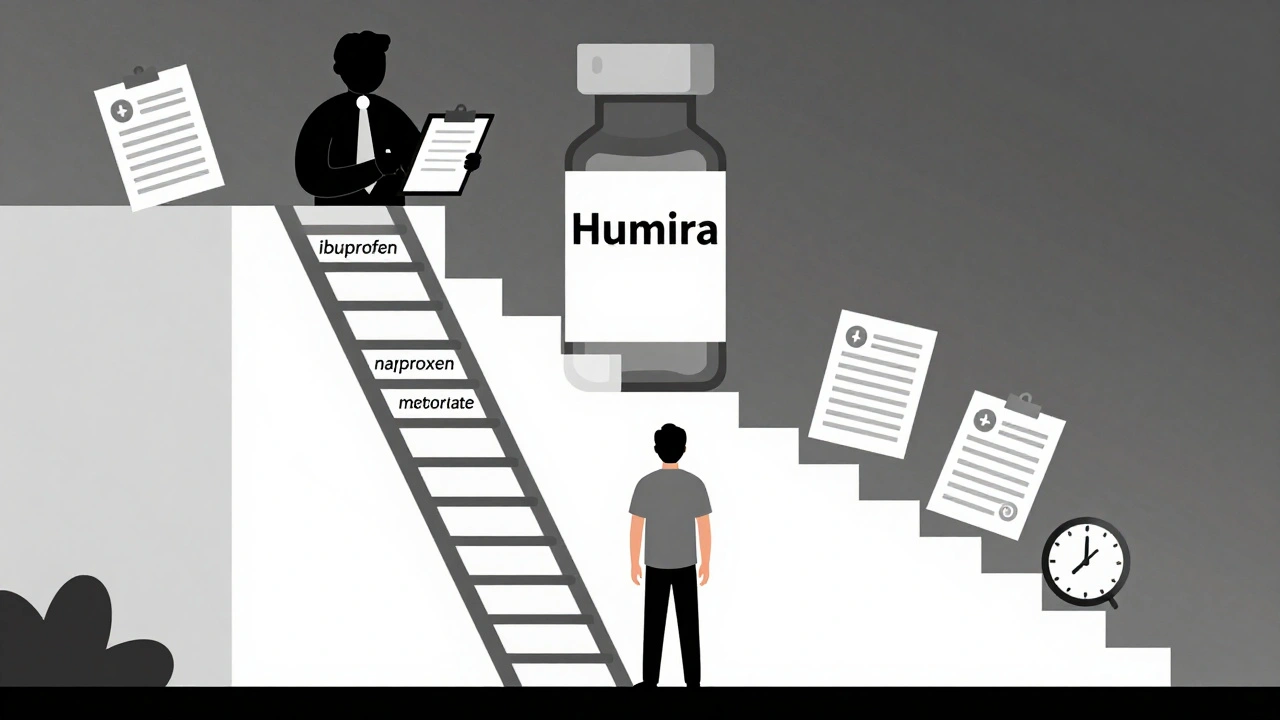
Step therapy forces patients to try cheaper generic drugs before insurers cover more expensive treatments. Learn how it works, when it fails, and what you can do to get exceptions quickly.
Drug Prior Authorization: What It Is, Why It Happens, and How to Navigate It
When your doctor prescribes a medication but your pharmacy says drug prior authorization, a process where insurance companies require approval before covering certain prescriptions. Also known as prior auth, it's not a delay tactic—it’s a cost-control step built into most health plans. But for patients, it often feels like a roadblock between needing medicine and actually getting it.
This process touches nearly every part of the healthcare system. insurance prior auth, the formal request submitted by your doctor’s office to your insurer usually happens when a drug is expensive, has cheaper alternatives, or is flagged for overuse. pharmacy prior authorization, the step where the pharmacist flags the prescription for review is where you might hear, "We need to call your doctor." It’s not about the drug being unsafe—it’s about whether your plan considers it "medically necessary" under their rules. These rules change by insurer, by state, and even by the specific drug brand.
Some drugs almost always need prior auth: biologics for arthritis, specialty cancer meds, or high-cost ADHD pills. Others, like generic blood pressure drugs, rarely do. The real issue? The process isn’t standardized. One insurer might approve a drug in 24 hours. Another could take five days. And if your doctor’s office is understaffed, that form might sit for a week. Meanwhile, you’re out of pills, feeling worse, and stuck calling between work calls.
But there’s a way through it. Most people don’t realize they can ask their doctor to submit the prior auth form on the same day as the prescription. Some pharmacies have staff dedicated to chasing these down. And if your plan denies it? You have the right to appeal. You’re not just a patient—you’re an advocate. The posts below show you how real people and real pharmacies cut through the red tape: from how to spot when prior auth is being misused, to how hospitals choose which drugs require it, to what happens when insurance denies a life-saving drug. You’ll find stories from pharmacists who’ve caught errors, patients who beat denials, and doctors who’ve learned the shortcuts. This isn’t about paperwork. It’s about getting the medicine you need without losing your time, your money, or your peace of mind.