Biologic drugs are made from living cells, not chemicals, making them impossible to copy exactly. That’s why biosimilars aren’t generics - they’re highly similar versions that still require complex manufacturing and rigorous testing.
Biologics Manufacturing: How Complex Drugs Are Made and Why It Matters
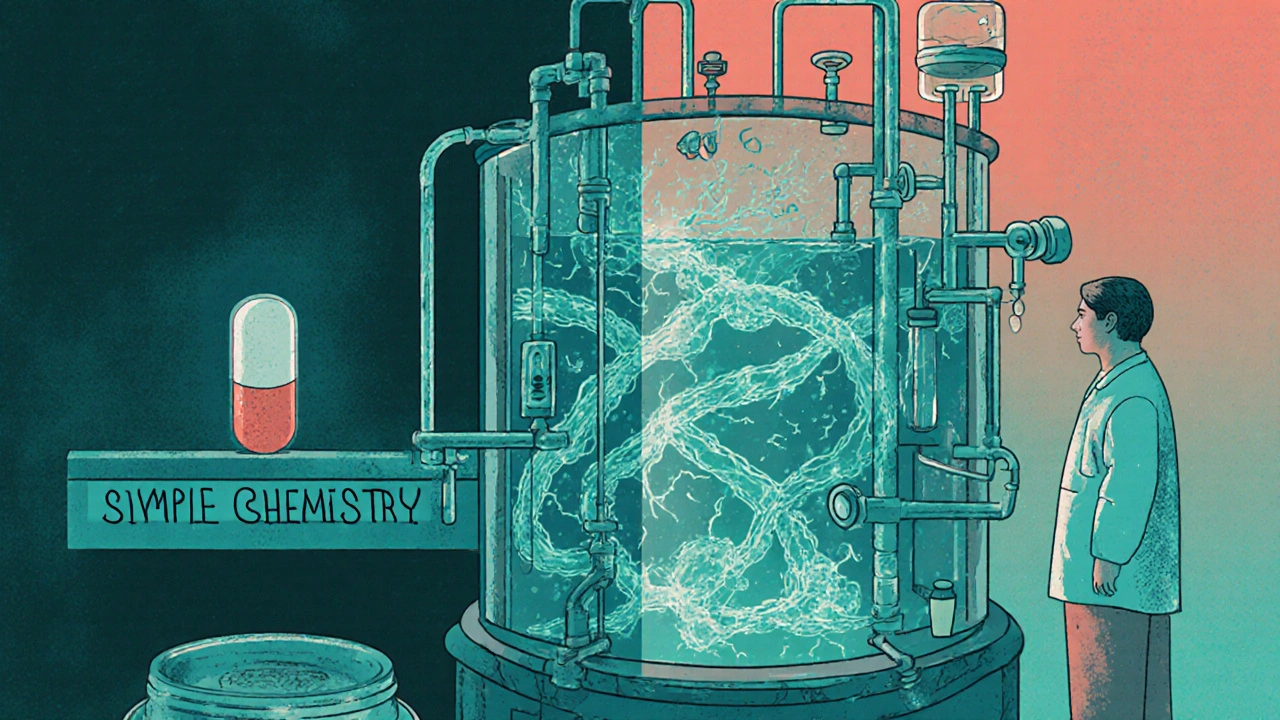
When you hear biologics manufacturing, the highly precise process of producing complex drugs derived from living organisms. Also known as biopharmaceutical production, it’s not like making aspirin in a lab. These drugs — think insulin, rheumatoid arthritis treatments, or cancer antibodies — are grown in living cells, not chemically synthesized. One tiny mistake in temperature, pH, or filtration can ruin an entire batch, making this one of the most demanding forms of drug production today.
Biologics manufacturing requires extreme control over every step: cell culture, purification, formulation, and packaging. Unlike small-molecule drugs, biologics are huge, fragile molecules that can change shape if handled wrong — and that change can turn a life-saving treatment into a dangerous one. That’s why regulatory approval, the strict oversight by agencies like the FDA and EMA to ensure safety and consistency. Also known as drug compliance, it’s non-negotiable in this space. Even small changes in the manufacturing process — like switching a filter or adjusting a stirrer speed — must be reported and approved. This is why posts on manufacturing changes and change control are so common in this field. A single unapproved tweak can trigger a product recall or legal action.
The rise of biosimilars, follow-on versions of biologics that must prove near-identical safety and effectiveness. Also known as biologic generics, they’re changing how healthcare systems manage costs has added another layer of complexity. Europe adopted biosimilars faster than the U.S., but recent regulatory shifts in 2024 are speeding up U.S. adoption. Still, proving two biologics are alike isn’t like proving two pills contain the same chemical. It requires thousands of tests — from protein folding to immune response — and even then, patients may react differently. That’s why posts on biosimilar regulation and biosimilar adoption keep popping up. It’s not just science — it’s economics, law, and patient safety all tangled together.
Behind every biologic is a team of engineers, biologists, and quality specialists working in sterile rooms, watching sensors, and documenting every move. The stakes are high: a single contaminated batch can cost millions and endanger lives. That’s why pharmaceutical quality, the system of controls ensuring every dose is safe, potent, and consistent. Also known as GMP compliance, it’s the backbone of this entire industry. You won’t find sloppy shortcuts here. Every step is tracked, validated, and audited. If you’ve ever wondered why biologics cost so much, this is part of the answer — it’s not just the research, it’s the relentless precision required to make them.
What you’ll find below are real, practical posts that dig into the details: how changes are approved, why biosimilars face different rules in Europe versus the U.S., how adverse reactions are tracked, and how hospitals decide which versions to use. These aren’t theoretical discussions — they’re the day-to-day realities for those who make, monitor, and prescribe these life-changing drugs. Whether you’re in pharma, healthcare, or just curious about how your medicine gets made, this collection gives you the real picture — no fluff, just facts.