When a spinal cord is injured, the body doesn’t just hurt-it loses control. Not just in the legs or arms, but in breathing, bladder function, temperature regulation, and even blood pressure. A spinal cord injury (SCI) isn’t a broken bone that heals. It’s a disruption in the body’s wiring, and the effects can be permanent. But here’s the truth: recovery isn’t about fixing the break. It’s about relearning how to live with what’s left. And with the right rehab and tools, many people rebuild lives that are full, active, and independent.
What Happens When the Spinal Cord Is Damaged
The spinal cord is your body’s main communication line. It carries signals from your brain to your muscles and organs, and back again. When it’s damaged-whether by a car crash, a fall, or a violent impact-those signals get cut off. The higher the injury, the more of your body is affected. A C1-C4 injury can leave you unable to breathe on your own. A T12 injury might mean loss of leg movement but full arm control. The injury level tells you what’s lost, but not what’s possible.Not all injuries are the same. Complete injuries mean no signals pass below the injury site. You have no feeling or movement. Incomplete injuries mean some signals get through. That’s where hope lives. Studies show that 59% of people with incomplete paraplegia regain some walking ability, while only 1-3% of those with complete paraplegia do. That’s not just statistics-it’s someone’s first step after three years of not moving their legs.
Secondary problems creep in fast. Muscles shrink without use. Joints stiffen. Pressure sores form from sitting too long. Bladder and bowel control vanish, requiring strict routines that take up to 90 minutes a day. Spasticity-uncontrolled muscle tightening-affects up to 78% of people with SCI. And because the nervous system is messed up, your body can’t regulate heat or sweat properly. You might overheat in a mild room or freeze in a warm one.
Rehab Starts the Day You’re Stabilized
Rehab doesn’t wait for you to feel ready. It starts within 24 to 72 hours after your injury is medically stable. That’s when therapists begin passive stretching-moving your limbs for you-to keep joints from locking up. If you’re flaccid (limp), they do this once a day. If you’re spastic (tight), they do it two or three times. Every day. No exceptions.By week two, you’re working on sitting balance, transfers from bed to wheelchair, and breathing exercises. High cervical injuries need special attention to prevent pneumonia. Techniques like assisted coughing, chest percussion, and incentive spirometry cut pneumonia risk by 65%. That’s not a guess-it’s from clinical data at Spaulding Rehabilitation.
Most inpatient rehab programs require at least three hours of therapy, five days a week. That’s physical therapy, occupational therapy, speech therapy, psychology, and nursing-all working together. A neuropsychologist helps you cope with grief and identity loss. An occupational therapist teaches you how to dress, bathe, and eat with adaptive tools. A social worker connects you to housing, benefits, and peer support.
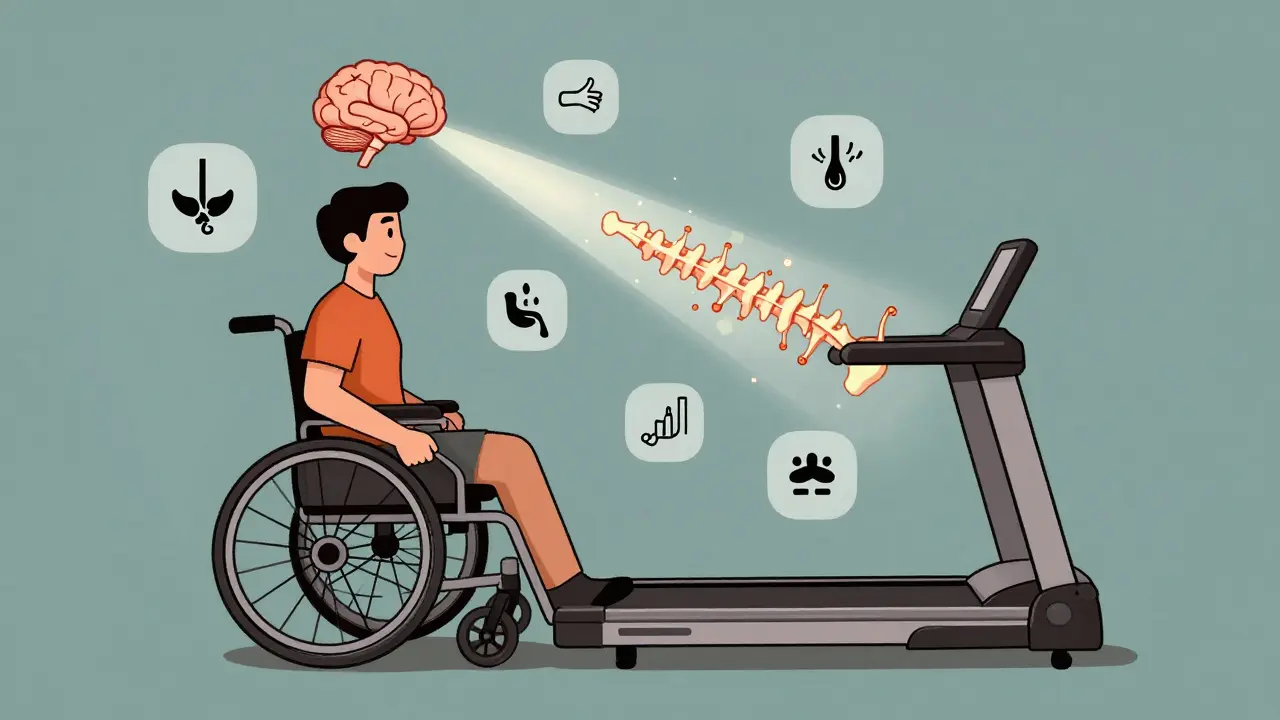
One of the most effective tools in modern rehab is treadmill training with body weight support. You’re suspended in a harness over a treadmill, and therapists help your legs move. It doesn’t look like walking. But it rewires your brain. Studies show it improves walking speed 23% more than regular overground walking. It’s not magic-it’s neuroplasticity. Your brain finds new paths when the old ones are blocked.

Assistive Devices: From Wheelchairs to Exoskeletons
You don’t have to be stuck in a chair. Assistive devices don’t just replace function-they restore dignity.Manual wheelchairs are still the standard. But they’re not one-size-fits-all. Custom seating systems prevent pressure sores and improve posture. Medicare covers 80% of the cost after your deductible, but the remaining $1,200 to $3,500 often comes out of pocket. Many people skip upgrades because they can’t afford them.
Power wheelchairs with head or sip-and-puff controls let people with high-level injuries move independently. Some even have tilt and recline features to manage spasticity and pressure.
Then there’s the newer tech: robotic exoskeletons like Ekso and ReWalk. These are motorized leg braces that let you stand and take steps. A user named ‘QuadLife2020’ on Reddit said his first steps in three years came from an Ekso session. But he also said the sessions were limited to 25 minutes because they drained his energy. And they’re expensive-$50,000 to $100,000. Insurance rarely covers them for home use.
Functional Electrical Stimulation (FES) is another game-changer. It sends small electric pulses to paralyzed muscles, making them contract. FES bikes let you pedal with your legs, even if you can’t move them yourself. One study showed FES cycling boosted oxygen use by 14.3%-nearly triple the gain from regular arm cycling. A user on the Christopher & Dana Reeve Foundation forum said FES helped him keep leg muscle mass after his T6 injury… but the $5,000 home unit was too much to pay alone.
For upper limbs, Armeo robotic arms help people relearn reaching and grasping. And now, the FDA has approved implantable diaphragm pacers for C3-C5 injuries. These devices stimulate the diaphragm, cutting ventilator dependence by 74%. That’s not a gadget-it’s freedom from a machine.
The Human Side of Recovery
Rehab isn’t just about muscles and machines. It’s about identity. Many people feel like they’ve lost themselves. Depression and anxiety are common. That’s why peer counseling is so powerful. At Spaulding, 82% of patients said talking to someone who’d been through it made them feel less alone.But support doesn’t last. A United Spinal Association survey found 68% of people quit their home exercise programs within six months. Why? No one checked in. No one reminded them. No one celebrated small wins. That’s the hidden gap in care.
And caregivers? They’re often overlooked. Improper transfers cause 32% of shoulder injuries in family members. Teaching caregivers how to lift, pivot, and support safely isn’t optional-it’s essential.
Documentation matters too. At top centers like Mayo Clinic, patients get over 100 pages of personalized rehab plans. At smaller clinics, they get a single pamphlet. The difference isn’t just paper-it’s outcomes.

What’s Next: AI, Brain Interfaces, and the Future
The field is changing fast. By 2025, 65% of leading rehab centers will use AI to tailor therapy plans based on your progress, muscle response, and even mood. It’s not sci-fi-it’s already happening.Brain-computer interfaces (BCIs) are in early trials. One study in Nature Medicine showed a 38% improvement in hand function for people with cervical injuries using BCIs. Imagine thinking about picking up a cup-and your hand moves, thanks to a tiny chip reading your brain signals.
But funding is a wall. Medicare pays only 83% of what it actually costs to run a rehab program. That means centers cut corners. New tech like exoskeletons and FES bikes sit unused because they’re too expensive to maintain.
And as the population ages, falls are rising. People over 65 are now getting spinal cord injuries from slips and stumbles at a rate of 4.2% per year. That’s a growing crisis-and a growing need for accessible, affordable rehab.
What You Can Do Right Now
If you or someone you love has a spinal cord injury:- Start rehab as soon as you’re cleared-don’t wait.
- Ask for a full team: physical, occupational, psychological, and social work support.
- Request FES or treadmill training if you have an incomplete injury.
- Get a custom wheelchair seating system-even if you have to fight for it.
- Connect with peer support groups. They’re not optional. They’re life-changing.
- Document everything. Keep a log of your progress, pain, and setbacks. Share it with your team.
- Know your insurance limits. Ask what’s covered and what’s not. Appeal denials.
Recovery isn’t linear. Some days you’ll feel like you’re moving forward. Others, you’ll feel stuck. That’s normal. The goal isn’t to walk again-it’s to live again. And with the right tools, the right people, and the right mindset, that’s possible.
Can you walk again after a spinal cord injury?
It depends on whether the injury is complete or incomplete. About 59% of people with incomplete injuries regain some ability to walk, especially with intensive rehab like treadmill training. For complete injuries, less than 3% regain walking ability. But walking isn’t the only measure of progress-many people use wheelchairs and still live full, active lives.
How long does spinal cord injury rehab last?
Rehab happens in phases. Acute rehab starts within days and lasts 6-12 weeks in a hospital. Subacute rehab continues for months with outpatient therapy. Long-term rehab can last years, focusing on adapting to life changes. Most people see the biggest gains in the first year, but improvements can continue for years with consistent therapy and exercise.
Are robotic exoskeletons worth it?
For some, yes. Exoskeletons like Ekso or ReWalk let people stand and take steps, which improves circulation, bone density, and mental well-being. But they’re expensive, require 2-3 therapists per session, and training is limited to 30-45 minutes. Most insurance won’t cover home use. They’re best for people with incomplete injuries who are motivated and have strong upper body strength.
What’s the best way to prevent pressure sores?
Change position every 15-30 minutes if you’re in a wheelchair. Use a custom cushion designed for SCI, check your skin daily for redness or warmth, and keep skin clean and dry. Avoid sitting on hard surfaces. If you notice a sore forming, see your doctor immediately-pressure sores can turn deadly fast.
Can I use FES cycling at home?
Yes, but it’s expensive. Home FES bikes cost around $5,000 and require a trained technician to set up. Medicare doesn’t cover them for home use. Some nonprofit groups and rehab centers offer loan programs. Talk to your therapist about options-many patients use them 3-5 times a week to maintain muscle and heart health.
How do I find a good rehab center?
Look for a facility that’s part of the Spinal Cord Injury Model Systems network-they meet the highest standards. Ask if they offer at least 3 hours of therapy daily, have a full team (including psychologists), and provide peer support. Check if they use evidence-based tech like FES or treadmill training. Don’t settle for a place that just gives you pamphlets.
What should I ask my insurance company?
Ask: What’s covered for inpatient rehab? Do you cover FES bikes, exoskeletons, or custom wheelchairs? What’s the limit on therapy visits per year? Do you cover home modifications? What’s the appeals process if they deny coverage? Write everything down. Many people get denied initially but win on appeal.
How do I help a loved one with SCI at home?
Learn proper transfer techniques-improper lifting causes shoulder injuries in caregivers. Help with daily routines like bladder care, skin checks, and stretching. Encourage movement, even small ones. Be patient. Listen more than you fix. And don’t forget to care for yourself-caregiver burnout is real.
Spinal cord injury changes everything-but it doesn’t define you. With the right support, technology, and persistence, people live rich, meaningful lives after SCI. The tools are here. The knowledge is here. What’s needed now is access, awareness, and the will to keep going.

Solomon Ahonsi
February 2, 2026 at 18:55This whole post reads like a pharmaceutical ad disguised as medical advice. Rehab? Sure. But who the hell can afford half this stuff? Exoskeletons for $100K? FES bikes that cost more than my car? And don't get me started on Medicare covering '83%' - that's just corporate speak for 'we're screwing you over.' You think people with SCI are just sitting around waiting for the next miracle device? Nah. They're stuck in a system that treats them like a line item on a balance sheet.
George Firican
February 3, 2026 at 01:21There's a quiet poetry in the way the body adapts when its wiring is severed - not as a failure, but as a reconfiguration. The spinal cord doesn't merely transmit signals; it's an archive of intention, a bridge between will and motion. When that bridge collapses, the brain doesn't surrender - it learns new dialects. Treadmill training isn't about walking again, it's about the nervous system whispering to itself in a different tongue. And yet, we measure progress in steps, not in the dignity of a person who learns to breathe without a machine, who dresses themselves with one hand, who laughs at a joke while their body betrays them. That's the real rehabilitation - not the hardware, but the human reclamation.
Matt W
February 3, 2026 at 09:27I’ve seen this firsthand with my cousin. He had a T6 injury. First six months were pure hell - depression, isolation, the whole thing. Then he got into FES cycling. Not because it was cool, but because his therapist didn’t give up on him. He started smiling again. Not because he could walk, but because he felt like he was doing something. That’s the part no one talks about - it’s not the tech that saves you, it’s the people who refuse to let you disappear.
Anthony Massirman
February 3, 2026 at 14:35Exoskeletons are cool but useless if you can’t afford them. End of story.
Monica Slypig
February 3, 2026 at 23:07Wow this is so typical of Canadian healthcare propaganda - pretending rehab is 'accessible' when in the US we actually have real innovation. You people just whine about cost while we're flying people to Houston for robotic gait training. And don't even get me started on how your 'peer support' is just people crying in a circle. We have AI-driven neurointerfaces here - not group hugs.
phara don
February 5, 2026 at 21:33Is there any data on long-term outcomes for people using home FES bikes? Like, after 5+ years? I’m curious if the muscle retention holds up or if it’s just a temporary boost. Also, how many users actually stick with it beyond the first year? Just wondering if the cost is worth the long-term ROI.
Hannah Gliane
February 6, 2026 at 08:53Oh wow 💖 so you're telling me that people with SCI are just supposed to 'live again' like it's a motivational poster? 🤦♀️ And let me guess - the answer is always 'get a custom wheelchair' - because clearly the problem is that they didn't buy the right $3,500 cushion. Meanwhile, their insurance denies everything and their caregiver just got a torn rotator cuff. Real inspiring. 😘
Murarikar Satishwar
February 6, 2026 at 13:05I come from a small village in India where spinal cord injuries often go untreated for months due to lack of access. But even here, families find ways - community support, homemade braces, neighbors helping with transfers. The tech you describe is incredible, but let's not pretend it's the only path to dignity. Human connection, patience, and persistence matter more than machines. We don't need a $50,000 exoskeleton to hold someone's hand while they learn to sit up again.
Dan Pearson
February 8, 2026 at 05:10Okay but let’s be real - this whole thing is just a glorified fundraising brochure for rehab centers. ‘AI-driven therapy plans’? Yeah right. They’re using a template from 2018. And ‘peer support changes lives’? Tell that to the guy who got kicked out of his rehab program because he ‘wasn’t motivated enough.’ Meanwhile, the CEO’s yacht is paid for by your donations. I’ve seen this script before. It’s not hope - it’s exploitation dressed in lab coats.
Bob Hynes
February 9, 2026 at 13:09Man I just flew back from Vancouver and saw this dude in a power chair with a head array controlling his whole rig - like, no hands, just sip and puff - and he was laughing at a meme on his tablet while cruising down the street. I cried. Not because he was ‘overcoming’ - but because he just lived. No fanfare. No TED Talk. Just… being. That’s the real win. The tech? It’s just the tool. The person? That’s the revolution.
Gary Mitts
February 10, 2026 at 09:50They say rehab starts in 24 hours but good luck getting a bed in a real facility. Wait times are 3 months in most states. Meanwhile your muscles are turning to jelly and your family is broke. This whole post feels like it was written by someone who’s never had to fight for care
clarissa sulio
February 11, 2026 at 22:07I'm so glad we're finally talking about this. My brother had a C5 injury and the only thing that helped was getting a diaphragm pacemaker. Now he breathes on his own. That’s not a gadget - that’s a miracle. And yes, insurance denied it twice. We appealed. We won. Don’t give up.
Bridget Molokomme
February 13, 2026 at 17:48So let me get this straight - you’re telling me the solution to a life-altering injury is… more paperwork? More appeals? More begging insurance companies? Wow. What a revolutionary insight. I bet the people who actually live this just sit around waiting for someone to write a pretty blog post about their suffering. So thoughtful.