It’s easy to assume that if you break out in hives after eating or taking something, it’s an allergy. But not all reactions are the same. Food allergies and medication allergies may look similar on the surface-itching, swelling, rash, trouble breathing-but they’re fundamentally different in how they happen, when they show up, and how they’re diagnosed. Mixing them up can lead to dangerous mistakes: avoiding life-saving antibiotics or eating something that triggers anaphylaxis. Knowing the difference isn’t just helpful-it can save your life.
How Your Body Reacts: Immune System Differences
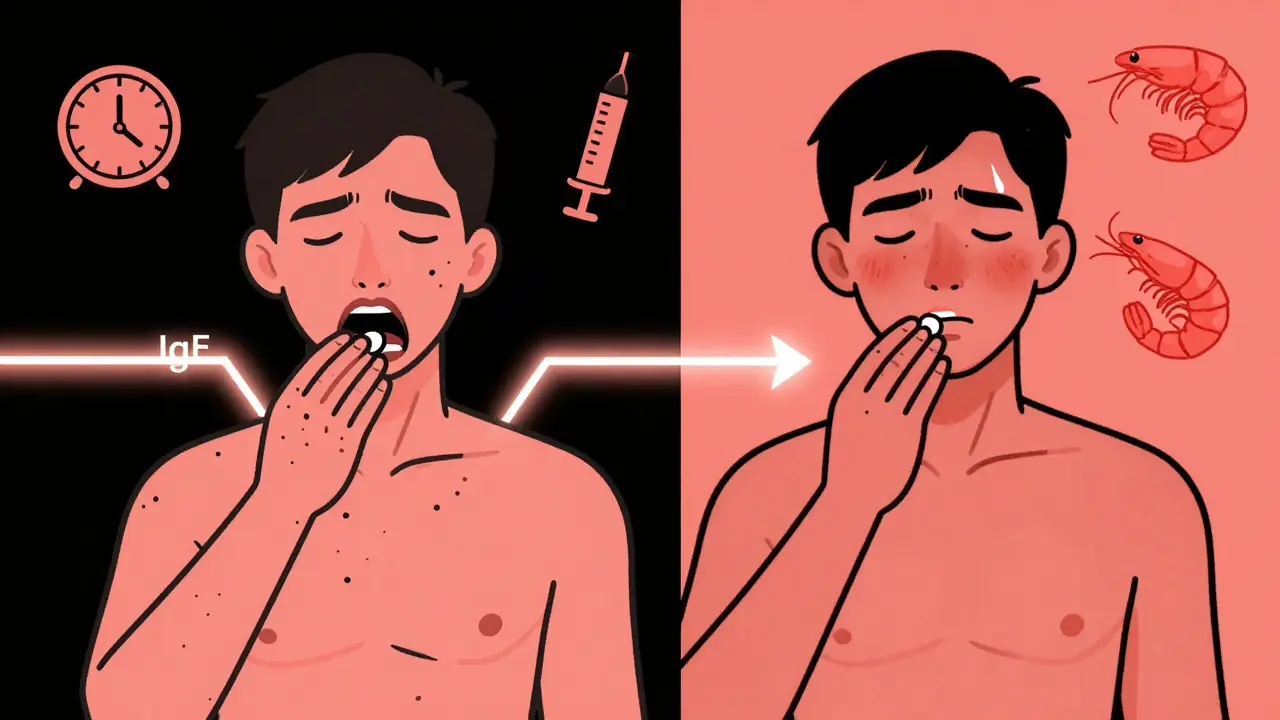
Food allergies almost always involve IgE antibodies. When you eat something you’re allergic to-like peanuts, milk, or shellfish-your immune system sees it as an invader and releases histamine and other chemicals. That’s what causes the quick symptoms: tingling lips, swelling, vomiting, or sudden difficulty breathing. About 90% of serious food reactions work this way. The rest, like FPIES (a severe gut reaction in babies), don’t involve IgE but still trigger the immune system in a delayed, non-IgE way. Medication allergies are more complex. About 80% of immediate reactions (like hives after penicillin) are IgE-mediated, just like food. But the other 20%? Those are T-cell driven and show up days or even weeks later. Think of a rash from amoxicillin that doesn’t appear until day 5. That’s not an IgE reaction. It’s a delayed immune response, often linked to viral infections like mononucleosis. This is why people get mislabeled as allergic to penicillin after a rash during a cold-when it was the virus, not the drug.Timing: When Symptoms Show Up
Food allergy symptoms hit fast. In 95% of cases, they start within 2 hours-often within 20 minutes. If you eat shrimp and your throat closes up 10 minutes later, that’s a classic IgE-mediated food reaction. The timing is predictable and repeatable. Eat it again? Same result. Medication reactions? Not so simple. Immediate reactions (hives, swelling, low blood pressure) can happen within minutes, just like food. But delayed reactions are common-and misleading. A rash from an antibiotic might not appear until 3 to 7 days after you started taking it. That’s why people think, “I’ve taken this before and was fine.” But now, with a virus or a different dose, your body reacts differently. That’s not a fluke. It’s a delayed immune response.Symptoms: What to Look For
Food allergies often include oral symptoms: itching or swelling in the mouth, lips, or throat. That’s called oral allergy syndrome. You might also get vomiting, diarrhea, or stomach cramps. Skin reactions like hives are common too-but they’re usually part of a broader system-wide response. Medication allergies are more likely to cause widespread rashes, especially maculopapular ones (flat red spots with bumps). Fever, swollen lymph nodes, and joint pain are more common with drug reactions than food reactions. Respiratory symptoms like wheezing happen in both, but in medication cases, they’re often tied to systemic involvement like DRESS syndrome or serum sickness-conditions that affect organs beyond the skin. One key difference: food allergies rarely cause prolonged fever or organ damage. Medication allergies can. If you develop a fever, liver problems, or kidney issues after taking a drug, that’s a red flag for a true drug hypersensitivity-not a food allergy.
Diagnosis: How Doctors Tell Them Apart
For food allergies, skin prick tests and blood tests for IgE antibodies are the first steps. But they’re not perfect. A positive test doesn’t always mean you’ll react when you eat the food. That’s why an oral food challenge-the gold standard-is often needed. You eat tiny, increasing amounts under medical supervision. If you react, you know for sure. Medication allergies are trickier. For penicillin, skin testing followed by an oral challenge is 99% accurate at ruling out true allergy. But for most other drugs-like NSAIDs, sulfa drugs, or chemotherapy-there’s no reliable blood or skin test. Doctors rely on detailed history, timing, and sometimes a controlled drug provocation test. Many people are labeled allergic based on a rash they had years ago, but 90% of those claims don’t hold up under testing. A 2022 JAMA study found that 85% of adults who say they’re allergic to penicillin aren’t truly allergic when tested. That means they’re avoiding a safe, cheap, effective antibiotic and instead getting broader-spectrum drugs that cost more and increase the risk of deadly infections like C. diff.Common Misconceptions and Real Stories
One of the biggest mistakes is confusing intolerance with allergy. Lactose intolerance causes bloating and diarrhea-but no immune response. It’s not dangerous. A true milk allergy can cause anaphylaxis. Yet, many people think they’re allergic because they get stomach upset after dairy. They’re not. They’re intolerant. Another common mix-up: rashes from viruses. Kids often get a rash after taking amoxicillin during a cold. Parents assume it’s a penicillin allergy. But if the child takes penicillin again without a virus, they may have no reaction at all. That’s not an allergy-it’s a coincidental rash. On the flip side, many people dismiss food allergy symptoms as “just indigestion.” A woman in Melbourne thought her nightly stomach cramps after eating eggs were just a sensitive stomach. She didn’t realize she was having mild anaphylaxis until she collapsed after a birthday cake. That’s why keeping a food-symptom diary matters. Write down what you ate, when, and exactly what happened-and how long it took.

Herman Rousseau
December 22, 2025 at 07:15Just had a friend get misdiagnosed with penicillin allergy after a rash during mono. Turned out she could take it just fine years later. Testing saved her from being stuck with expensive, toxic alternatives. Seriously, if you think you’re allergic to a drug, get tested. It’s not just about saving money-it’s about saving your life.
And yes, I’m a pharmacist. This isn’t opinion. This is data.
Ajay Brahmandam
December 23, 2025 at 09:03My kid broke out in hives after eating peanut butter at daycare. We panicked, went to the allergist, got tested. Turns out it was a mild IgE thing. We avoided peanuts for a year, did a supervised challenge, and now he eats them like popcorn. Don’t assume the worst. Get the facts.
Art Van Gelder
December 24, 2025 at 19:49Think about it-our immune system is basically a paranoid security guard who got trained by a 1980s action movie. It sees a peanut, screams ‘TERRORIST!’ and launches a full-scale assault. But then it sees amoxicillin, shrugs, and says ‘eh, maybe it’s just the flu’... until three days later, when it drops a full-blown rash like it’s dropping a mic.
We treat allergies like they’re simple switches-on or off-but the body? It’s a symphony of chaos. One note out of place and the whole thing collapses. We label people ‘allergic’ like it’s a tattoo, but sometimes it’s just a temporary glitch in the matrix. The real question isn’t what’s wrong with the body-it’s what’s wrong with how we diagnose it.
Jeremy Hendriks
December 26, 2025 at 16:57You people act like this is some deep mystery. It’s not. Food allergies kill fast. Drug allergies kill slow and quietly. One makes you scream, the other makes you die in a hospital bed because your doctor didn’t believe you. Stop romanticizing it. Stop calling it ‘interesting.’ It’s a fucking death sentence if you get it wrong.
Candy Cotton
December 28, 2025 at 00:37It’s ridiculous how many Americans self-diagnose allergies. I’ve seen people avoid gluten because they had a stomach ache once. Meanwhile, in India, we don’t have this culture of panic. We trust our doctors. We don’t turn every burp into anaphylaxis. This article is good, but it’s also a symptom of American medical overreach.
Tarun Sharma
December 28, 2025 at 09:34Respectfully, the distinction between IgE-mediated and T-cell-mediated reactions is critical for clinical decision-making. Misclassification leads to inappropriate avoidance and increased antimicrobial resistance. I recommend all patients with suspected drug hypersensitivity be referred to immunology for structured evaluation.
jenny guachamboza
December 28, 2025 at 20:24ok so like... what if the REAL problem is that our bodies are just full of toxins from the food industry?? like maybe we’re not allergic to peanuts... maybe we’re allergic to MONSANTO?? 🤔 maybe penicillin is just the last straw?? 🤯 also i think the FDA is lying to us about vaccines?? 🍎💊 #truth
Jim Brown
December 30, 2025 at 13:29There is, in the architecture of human physiology, a profound irony: we have evolved to detect and destroy foreign agents with astonishing precision, yet we remain utterly incapable of distinguishing between the signal and the noise-between the true threat and the phantom. The immune system, in its noble fidelity, becomes a tyrant of misinterpretation. A rash on day five is not a betrayal-it is a whisper from the body, too subtle for the hurried physician, too complex for the hurried mind. To label is to simplify. To know is to suffer the ambiguity. And perhaps, in that ambiguity, lies our only true salvation.
Sai Keerthan Reddy Proddatoori
January 1, 2026 at 01:48US doctors are just selling fear to make money. In India, we don’t need all these tests. If you feel sick after eating something, you stop eating it. Simple. No blood tests. No challenges. No expensive hospitals. This whole thing is a capitalist scam. Also, why are so many Americans allergic to everything? It’s because they eat processed garbage. Eat real food. Stop being weak.
Johnnie R. Bailey
January 1, 2026 at 09:34One thing no one talks about: cross-reactivity. If you’re allergic to birch pollen, you might react to apples, carrots, or almonds. That’s oral allergy syndrome. It’s not a true food allergy-it’s a molecular mix-up. Same with shellfish and dust mites. The immune system sees similar proteins and goes haywire. This isn’t about ‘being allergic to food.’ It’s about your immune system being confused by evolution’s sloppy design. Testing helps, but understanding the ‘why’? That’s the real liberation.
Nader Bsyouni
January 2, 2026 at 07:13Everyone talks about IgE and T-cells like they’re some profound revelation. Newsflash: medicine is a religion. The allergist is the priest. The skin test is the sacrament. The oral challenge? The holy communion. You don’t question it. You bow. You pay. You believe. The science is just the incense they burn to make you forget that nobody really understands why your body hates peanut butter.
Vikrant Sura
January 2, 2026 at 15:31Interesting. But I’ve read better.
Julie Chavassieux
January 3, 2026 at 03:37My sister had a rash after amoxicillin. She was labeled allergic. Never tested. Now she can’t get antibiotics for UTIs. She’s had three kidney infections. They could’ve avoided it all. Just one test. One hour. But no. They just wrote it down and moved on. People die from this. Not because of allergies. Because of laziness.
Kathryn Weymouth
January 3, 2026 at 19:17Thank you for this. I’m a nurse who’s seen too many patients avoid penicillin because of a childhood rash. One man, 72, had a C. diff infection after being given vancomycin because he was ‘allergic’-when he’d never actually been tested. He recovered after a supervised challenge. He cried. He said, ‘I’ve been scared of this drug for 50 years.’ That’s not just medical error. That’s a life stolen by misinformation.