Over 1 in 5 people worldwide have a fungal skin infection right now. It’s not rare. It’s not exotic. It’s not just a "bad case of itch"-it’s a real, common, and often misunderstood problem. You might think it’s just from being sweaty or not washing enough, but the truth is more complicated. Fungal skin infections like Candida and ringworm behave differently, need different treatments, and can easily be mistaken for something else-like eczema or psoriasis. If you’ve ever had a red, itchy patch that won’t go away, or a rash that comes back every summer, you’re not alone.
What Exactly Is Ringworm?
Ringworm isn’t caused by a worm. That’s the first thing to clear up. The name comes from the old-school way doctors described it: a circular, red, scaly patch with a raised edge and clearer center-like a worm curled up under the skin. But it’s actually a group of fungi called dermatophytes. These fungi feed on keratin, the same protein found in your skin, hair, and nails. That’s why they love the scalp, feet, groin, and under the nails.
The most common culprit is Trichophyton rubrum, responsible for 80-90% of cases. You can catch it from walking barefoot in a locker room, sharing a towel, or petting a dog with a patchy coat. Kids are especially vulnerable-tinea capitis (scalp ringworm) is one of the top fungal infections in children under 12. In adults, tinea pedis (athlete’s foot) and tinea cruris (jock itch) are more common. The infection spreads easily in warm, damp places. If you’ve ever had a rash between your toes that peels and stings, that’s likely ringworm.
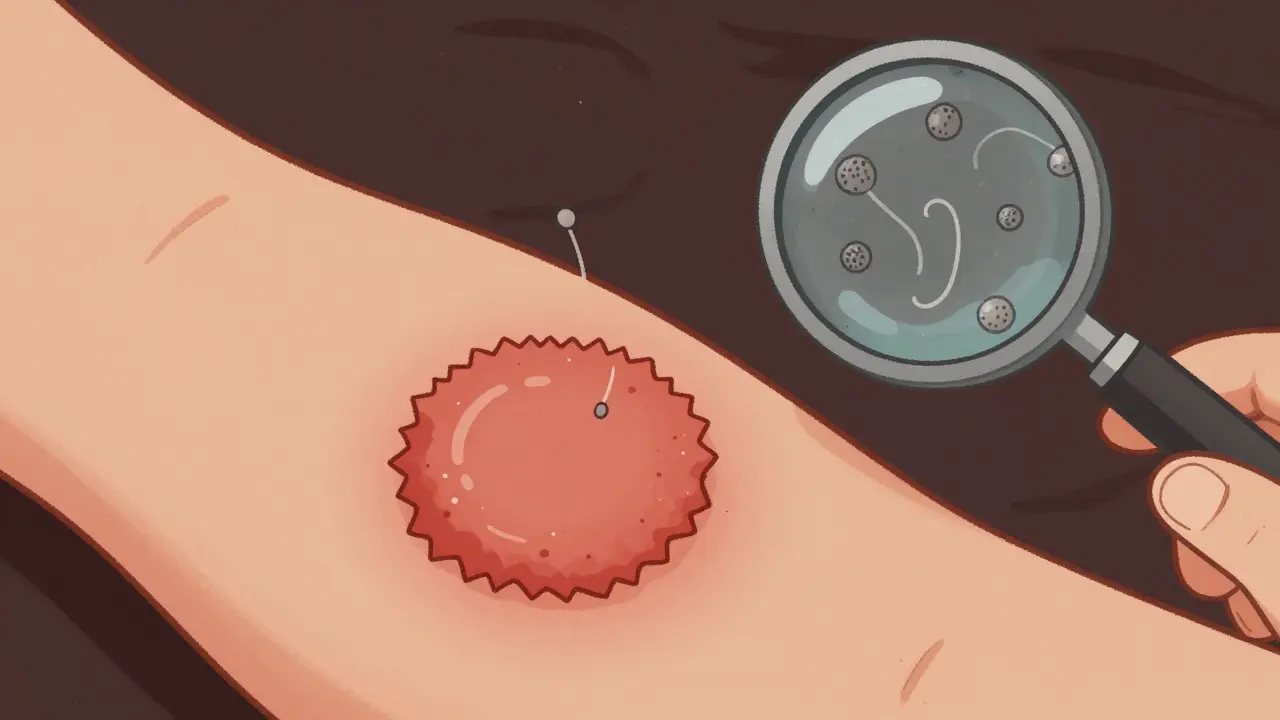
The classic sign? A red, circular patch with a defined, scaly border. It often itches. Sometimes it blisters. It doesn’t always look like a perfect circle-especially on darker skin tones. That’s why many people think it’s just a bad rash and wait too long to treat it. Left untreated, it can spread to nails or even other parts of the body.
What About Candida?
While ringworm is caused by mold-like fungi, Candida is yeast. It’s a type of fungus that lives on your skin and inside your body-normally harmless. But when things get out of balance, it overgrows. Warm, moist areas are its favorite spots: under the breasts, in skin folds, in the groin, and around the diaper area in babies. It doesn’t form rings. Instead, it looks like a bright red, wet-looking rash with tiny red bumps around the edges-called satellite pustules.
Candida albicans is the usual offender. But in recent years, other strains like Candida auris have started showing up in hospitals. This one’s scary because it’s resistant to multiple antifungal drugs and can stick to skin for weeks, spreading between patients. It’s still rare in healthy people, but for those with diabetes, weakened immune systems, or who use long-term antibiotics, the risk jumps.
In babies, diaper rash from Candida doesn’t respond to regular zinc oxide creams. It’s deeper red, often with white patches or pus-filled spots. In adults, especially women, recurrent vaginal yeast infections are often linked to the same Candida species. Many people don’t realize these are fungal infections too. And yes, they can spread to the skin around the genitals.
How Do You Know Which One You Have?
Here’s where things get tricky. Both can look similar: red, itchy, flaky. But the clues are there if you know what to look for.
- Ringworm: Clear center, raised border, dry scales, often circular. Common on arms, legs, face. Can affect nails-thick, yellow, crumbling.
- Candida: Moist, beefy red, no clear center, small red bumps around the edges. Found in skin folds, under breasts, in groin, diaper area.
Doctors often use a quick test: scraping a bit of skin and looking at it under a microscope with potassium hydroxide (KOH). That kills off human cells and lets the fungal threads show up. It’s fast, cheap, and works about 70-80% of the time. If it’s not clear, they might send a culture-but that takes weeks.
Here’s the problem: primary care doctors miss the diagnosis up to half the time. A 2022 study showed dermatologists get it right 85-90% of the time. Most people end up using steroid creams thinking it’s eczema-only to make it worse. Steroids suppress the immune response, letting the fungus spread faster. That’s why some rashes seem to get worse after using hydrocortisone.

What Treatments Actually Work?
Not all antifungals are the same. And not all over-the-counter creams are equal.
For ringworm on the skin (tinea corporis), topical treatments like terbinafine (Lamisil) or clotrimazole (Lotrimin) work well. Apply twice daily for 1-2 weeks. Studies show 70-90% cure rates. But you have to keep using it even after it looks better. Stopping early is the #1 reason it comes back.
For nail infections (tinea unguium), topical creams don’t cut it. The fungus hides deep under the nail. You need oral medication-usually terbinafine for 6-12 weeks. It’s effective in 80-90% of cases, but liver enzymes need checking. Some people get a mild upset stomach or headache. It’s not dangerous for most, but if you have liver disease, your doctor will avoid it.
For Candida, topical azoles like clotrimazole or miconazole are first-line. Apply once or twice daily for 1-2 weeks. Nystatin is another option, especially for babies. If it’s severe, or if it keeps coming back, oral fluconazole is used. But here’s the catch: fluconazole resistance is rising. A 2023 study found some Candida strains are now resistant in over 10% of cases.
There’s a new drug on the market: ibrexafungerp (Brexafemme). Approved in 2023 for recurrent vaginal yeast infections, it’s the first new class of antifungal in years. It works differently and may help where others fail. But it’s not for skin rashes yet.
Why Do These Infections Keep Coming Back?
Recurrence is the biggest frustration. One in three people who’ve had a fungal skin infection get it again within a year. Why?
- Incomplete treatment: Stopping when it looks better, not when it’s gone.
- Re-exposure: Walking barefoot in the same shower, sharing towels, or petting an infected dog.
- Underlying conditions: Diabetes, obesity, or a weakened immune system make you more prone.
- Moisture: Not drying skin folds after showering, wearing tight synthetic underwear, or sweating all day.
People with diabetes are 2.5 times more likely to get fungal infections. High sugar levels feed the yeast. If you have recurring rashes and you’re diabetic, controlling blood sugar is as important as the cream you use.
There’s also growing evidence that probiotics help. A 2023 survey of 850 people found that 65% who took Lactobacillus supplements while using antifungals had fewer recurrences. It’s not a cure, but it might help tip the balance back in your favor.
What’s New in the Fight Against Fungi?
The battle is changing. Fungal resistance is rising. Terbinafine resistance in Trichophyton rubrum is now seen in 5-7% of cases in North America. Candida auris is spreading in hospitals, and it’s often resistant to multiple drugs.
New antifungals are in the pipeline. Olorofim, a drug in late-stage trials, shows promise against resistant strains. The NIH has poured $32 million into fungal microbiome research-studying how good bacteria might keep bad fungi in check.
Guidelines are also shifting. The American Academy of Dermatology now advises against using oral antifungals for simple ringworm on the skin. Topical creams are just as effective and carry far less risk. They also recommend ciclopirox over selenium sulfide for tinea versicolor, because it works better.
And the market is responding. Over-the-counter antifungal sales hit $1.8 billion in the U.S. in 2022. Terbinafine and clotrimazole dominate. But more people are asking for alternatives-natural oils, probiotics, better hygiene routines. The old approach of "just use the cream" isn’t enough anymore.
What Should You Do Right Now?
If you have a persistent rash:
- Don’t use steroid creams unless a doctor says so. They can make fungal infections worse.
- Try an OTC antifungal cream with terbinafine or clotrimazole. Apply twice daily for at least two weeks-even if it looks better in three days.
- Keep the area clean and dry. After showering, pat skin folds dry. Wear cotton underwear. Avoid tight clothes.
- If it doesn’t improve in 2 weeks, or if it spreads, see a doctor. Ask for a KOH test.
- If you have diabetes, check your blood sugar. High levels are fueling the infection.
- If it keeps coming back, talk about probiotics. Lactobacillus strains may help prevent recurrence.
Fungal skin infections aren’t embarrassing. They’re common. They’re treatable. But they won’t go away if you ignore them-or if you treat them wrong. The right treatment, applied correctly, works. And you don’t need a prescription for most cases. Just the right knowledge.

James Rayner
December 15, 2025 at 17:20Wow. This is the most clear-headed breakdown of fungal infections I’ve ever read. I used to think ringworm was just a myth from old cartoons. Now I know why my cousin’s rash kept coming back after steroid cream. Thanks for the KOH test tip-so many docs skip that.
Kim Hines
December 16, 2025 at 17:08I had a rash under my breast for months. Thought it was heat rash. Turns out it was Candida. This post saved me.
sue spark
December 18, 2025 at 14:06I never realized how much sugar feeds these infections. I’ve been diabetic for 12 years and had the same rash every summer. I’m gonna try the probiotics and cut back on sweets. Hope it works
Mike Smith
December 20, 2025 at 12:00Thank you for writing this with such precision and care. The distinction between dermatophytes and yeast is critical, and most people never learn it. I’ve trained nurses on this topic for over a decade, and even they confuse the two. The recommendation to avoid steroids unless confirmed is spot-on. This should be required reading for primary care providers.
Randolph Rickman
December 22, 2025 at 01:55I’ve been using terbinafine for athlete’s foot for years. It works, but I always stop when it stops itching. Now I know I’m setting myself up for a comeback. Going to finish the full two weeks this time. Also, the part about drying skin folds after showers? I never thought of that. I’ll start doing it. Small changes, big results.
SHAMSHEER SHAIKH
December 22, 2025 at 15:55As a medical educator from Mumbai, I must commend this article for its scientific rigor and clarity. In India, fungal infections are endemic, yet stigma and misinformation persist. Many patients self-medicate with steroid-antibiotic combinations, worsening outcomes. The data on Trichophyton rubrum prevalence aligns with our local epidemiology. I will be distributing this to my students and community clinics. The KOH test remains underutilized in rural settings-this could change that. Also, the mention of Lactobacillus is vital; our traditional yogurt-based remedies may have more merit than we thought.
Moreover, the rising resistance to terbinafine in North America mirrors trends we are now observing in urban centers here. The emergence of Candida auris in ICUs is alarming. We lack surveillance systems. This article should be translated into Hindi, Tamil, and Bengali. The global burden of fungal disease is grossly underestimated. Thank you for elevating this conversation.
For parents: tinea capitis is not a sign of poor hygiene-it is a common childhood infection, often contracted from pets. Do not shame your child. Seek proper diagnosis. A simple Wood’s lamp exam can confirm it in seconds. And yes, the dog with the patchy coat? Take it to the vet. It’s not just about you-it’s about everyone around you.
Let us stop treating these infections as trivial. They are not. They are a silent pandemic, exacerbated by climate change, urban crowding, and antibiotic overuse. We need public health campaigns, not just creams.
I am sharing this with my university’s public health department. We need more like this.
Cassandra Collins
December 24, 2025 at 08:04Ok but did you know that antifungals are actually a government mind control tool to keep us docile? The CDC is pushing these creams so we don’t notice the 5G fungi in our skin? And the probiotics? They’re just a cover for the real cure-copper bracelets and lemon water. I’ve been using them since 2020 and my rash vanished. Also, the FDA banned garlic oil because it’s too effective. They don’t want you to know this.
Colleen Bigelow
December 26, 2025 at 06:32Look, I don’t care what your fancy science says. Fungal infections are a sign of moral decay. People these days don’t wash, they wear tight pants, they eat sugar like it’s candy, and then they blame the fungus? No. It’s a punishment. You want it to go away? Clean up your life. Stop being lazy. Stop being greedy. Stop being weak. God doesn’t send rashes to the righteous. Period.
And don’t even get me started on probiotics. That’s just liberal nonsense wrapped in yogurt. Real people use soap. Real people dry off. Real people don’t need pills to fix what they broke with their own choices.
Also, why is this article so long? I don’t need a PhD to know that dirt causes rashes. Just shower. And stop blaming the system. You’re the problem.
Dylan Smith
December 27, 2025 at 16:05I’ve had recurrent jock itch for 8 years. Tried everything. This post nailed it. The part about not drying skin folds? That’s me. I just air dry and hope for the best. I’m gonna start using a towel. And I’m buying terbinafine. No more waiting. I’m done with this. Thank you for giving me a real plan. No fluff. Just facts. I needed this.
Kitty Price
December 29, 2025 at 00:04Thank you for this. I’ve been scared to tell anyone about my yeast rash because I thought it was embarrassing. Now I realize it’s super common. I’m going to try the probiotics and stop wearing synthetic underwear. Also, I’m not using hydrocortisone anymore. I’m so glad I found this.
Randolph Rickman
December 30, 2025 at 14:28Just read the comment from Shamsheer. That was incredible. You just turned a medical article into a public health manifesto. I’m printing this out for my clinic. We need more people like you who see the bigger picture. Thank you for the global perspective.