Over 19% of adults in the U.S. experience an anxiety disorder each year. That’s nearly 1 in 5 people. Many of them don’t realize what they’re feeling isn’t just stress-it’s a medical condition. Anxiety disorders aren’t about being nervous before a presentation or worrying about bills. They’re persistent, overwhelming, and often paralyzing. The fear doesn’t fade. The racing heart doesn’t stop. The thoughts loop like a broken record. And for too long, people have been told to just relax, breathe, or snap out of it. But anxiety disorders don’t respond to willpower. They respond to science.
What Are the Main Types of Anxiety Disorders?
- Generalized Anxiety Disorder (GAD) - This is the most common form. People with GAD worry constantly about everyday things-work, health, family, even minor decisions. The worry isn’t proportional to the situation. It’s relentless, lasting six months or more. You might feel on edge all the time, even when nothing is wrong.
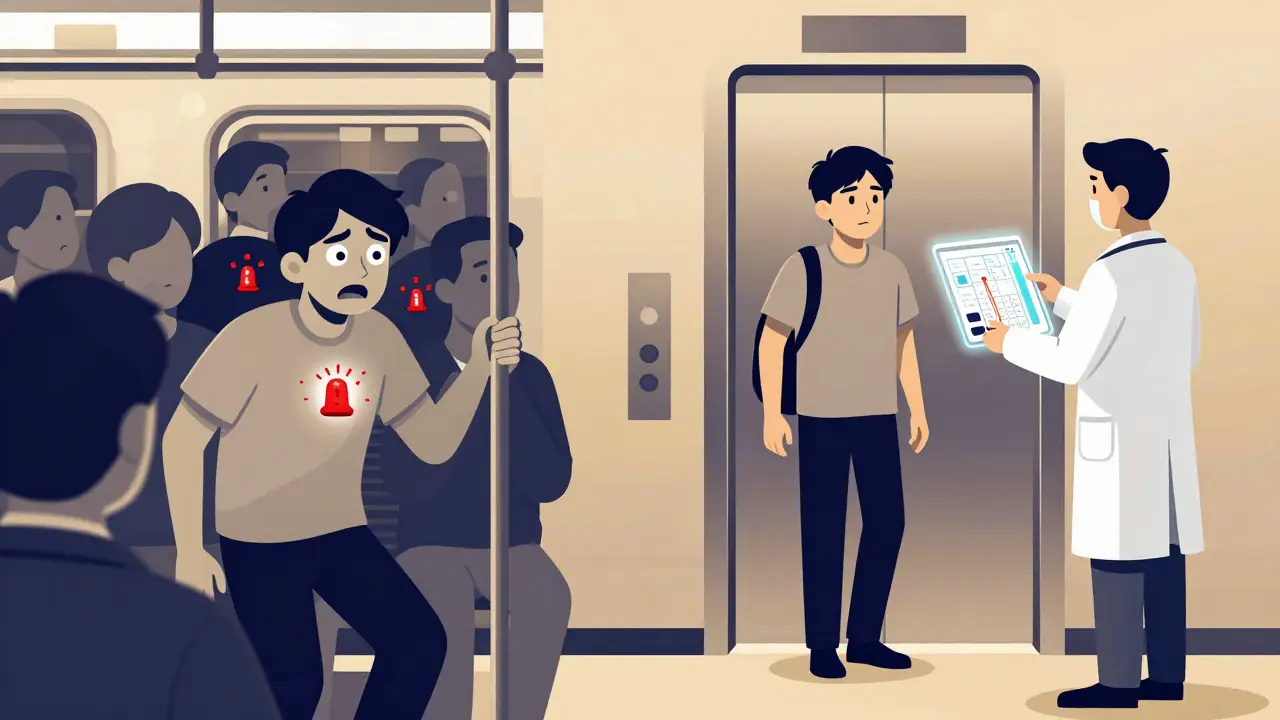
- Panic Disorder - Sudden, intense surges of fear that come out of nowhere. These are panic attacks. They hit hard: chest pain, dizziness, shaking, shortness of breath, and the terrifying belief that you’re dying or losing control. After one attack, many people live in fear of the next one, avoiding places or situations where they feel unsafe.
- Social Anxiety Disorder - It’s not just shyness. This is a deep fear of being judged, embarrassed, or humiliated in social settings. Talking to coworkers, eating in public, or even making eye contact can trigger extreme discomfort. Some people avoid social events altogether.
- Specific Phobias - An intense, irrational fear of a specific object or situation-heights, spiders, flying, needles. The fear is so strong that people go out of their way to avoid it, even if it disrupts their life. A fear of flying might mean missing a family reunion. A fear of needles could mean avoiding necessary medical care.
- Obsessive-Compulsive Disorder (OCD) - Though now classified separately, OCD still shares roots with anxiety disorders. It involves unwanted, intrusive thoughts (obsessions) and repetitive behaviors (compulsions) meant to reduce the anxiety they cause. Washing hands dozens of times, checking locks repeatedly, mentally reviewing conversations-these aren’t quirks. They’re symptoms.
- Separation Anxiety Disorder - Often thought of as a childhood issue, this affects adults too. The fear of being separated from loved ones can be so severe that it prevents someone from leaving home, traveling, or even sleeping alone.
- Selective Mutism - Mostly seen in children, this is when someone can speak normally at home but remains silent in certain settings like school or with strangers. It’s not defiance-it’s extreme anxiety that freezes their voice.
Each of these has its own pattern, but they all share one thing: the brain’s alarm system is stuck on high. Even when there’s no real danger, the body reacts as if there is.
What Do Anxiety Symptoms Actually Look Like?
Anxiety doesn’t just live in your head. It lives in your body too.
Physical symptoms are common across all types:
- Heart rate spikes to 110-140 beats per minute during panic attacks
- Sweating (reported by 92% of those with panic disorder)
- Trembling or shaking (87%)
- Shortness of breath (83%)
- Dizziness or lightheadedness (76%)
- Nausea or stomach upset (68%)
Cognitive symptoms are just as disruptive:
- Racing thoughts (82%)
- Difficulty concentrating (89% in GAD)
- Catastrophic thinking (“What if I collapse right now?”)
- Rumination-replaying the same thought or situation over and over (91%)
Emotionally, people describe:
- A constant sense of impending doom (95% during panic attacks)
- Feeling like they’re losing control or going crazy (88%)
- Excessive worry that doesn’t match the actual risk (100% in GAD)
These aren’t random feelings. They’re measurable, repeatable responses tied to how the brain processes threat. The amygdala-the brain’s fear center-becomes hypersensitive. The prefrontal cortex, which normally calms things down, gets overwhelmed. That’s why telling someone to “calm down” rarely works. Their nervous system is running on autopilot.
What Treatments Actually Work?
There’s a lot of noise out there-supplements, crystals, detoxes, miracle cures. But the science is clear: only a few treatments have been proven to reduce anxiety symptoms over time.
Cognitive Behavioral Therapy (CBT) is the gold standard. It’s not talking about your past. It’s learning how your thoughts create your feelings, and how to change them. A typical CBT program lasts 12 to 20 sessions, each about an hour long. By session 12, 60-80% of people report meaningful improvement.
One of the most powerful tools in CBT is exposure therapy. For someone with a fear of elevators, that might mean starting by looking at pictures of elevators, then standing near one, then stepping inside for 10 seconds, then riding one floor. Each step is done slowly, safely, and repeatedly until the fear loses its power. Studies show exposure therapy works for 60-80% of people with social anxiety or specific phobias.
CBT isn’t just for therapy rooms. Digital tools like nOCD and Wysa are FDA-cleared and offer guided CBT exercises. In 8 weeks, users report 35-45% symptom reduction with just 20-30 minutes a day.
Medication is another proven option. SSRIs-like sertraline (Zoloft) and fluoxetine (Prozac)-are first-line choices. They don’t work instantly. It takes 6-12 weeks for full effect. But when they do, they reduce both emotional and physical symptoms. About 40-60% of people respond well. SNRIs like venlafaxine are also effective.
Benzodiazepines-like Xanax or Klonopin-give fast relief. But they’re not a long-term solution. They carry a 15-30% risk of dependence with regular use. They can also dull emotions, impair memory, and cause withdrawal symptoms. Most guidelines now recommend them only for short-term use during crises.
For treatment-resistant cases, newer options are emerging. In 2023, the FDA approved zuranolone (Zurzuvae), an oral neuroactive steroid for postpartum anxiety, with a 54% remission rate in trials. Research into ketamine-assisted therapy shows rapid response in 65% of treatment-resistant cases within hours.
Why Do So Many People Struggle to Get Help?
Even with proven treatments, only 37% of people with anxiety disorders achieve remission after six months of standard care. Why?
- Wait times for specialized therapists average 6-8 weeks. In rural areas, it’s longer.
- Cost and insurance limits often cap therapy sessions to 10-12 per year. Many can’t afford out-of-pocket costs.
- Side effects from medication can be worse than the anxiety itself-emotional numbness, weight gain, sexual dysfunction. Some people quit because they feel “not like themselves.”
- Exposure therapy is hard. It’s designed to make you uncomfortable. Many people drop out because it feels too scary at first.
- Stigma still exists. Some people feel ashamed to say they’re in therapy. Others believe they should be able to handle it on their own.
Real stories from online communities reflect this struggle. One user wrote: “CBT helped my panic attacks drop from 5-7 a week to 1-2. But the exposure exercises made me want to quit.” Another said: “SSRIs helped my body, but I felt like a zombie. Switched to buspirone-much better.”
Combining therapy and medication works best. A 2023 NAMI survey found 58% of people improved with both, compared to 42% with medication alone and 38% with therapy alone.

What’s New in Anxiety Treatment?
The field is moving fast. In 2023, researchers identified three distinct “anxiety biotypes” using brain scans. These patterns predict who will respond best to CBT versus medication. This is the beginning of personalized treatment.
AI is stepping in too. Stanford researchers built an algorithm that predicts panic attacks with 87% accuracy-24 hours in advance-by analyzing voice patterns, movement, and heart rate variability from smartwatches.
Acceptance and Commitment Therapy (ACT) is now recognized as a first-line treatment alongside CBT. Instead of fighting thoughts, ACT teaches you to notice them without judgment and take action aligned with your values. It’s less about “fixing” anxiety and more about living well despite it.
By 2030, genetic testing may guide medication choices with 70% accuracy, cutting out years of trial and error. Medicare now covers two CBT-based digital platforms, reimbursing $120-$180 per completed module. That’s a big step toward accessibility.
What Can You Do Right Now?
If you’re struggling:
- Track your symptoms. Use a simple journal: date, time, trigger, physical sensation, thought, and how you responded. Patterns will emerge.
- Practice diaphragmatic breathing. Breathe in slowly through your nose for 5 seconds, hold for 2, exhale through your mouth for 6. Do this 5 times, 3 times a day. It lowers your heart rate and signals safety to your brain.
- Try a digital CBT app. nOCD, Wysa, or Sanvello offer free trials. No waiting list. No cost upfront.
- Reach out. Call the NAMI Helpline (24/7) or join a local support group. You’re not alone. The Anxiety and Depression Association of America runs over 300 weekly support groups across the U.S.
- See a professional. Start with your primary care doctor. They can screen for anxiety and refer you to a therapist or psychiatrist. You don’t need to “be ready.” You just need to show up.
Anxiety disorders are not a weakness. They’re a misfiring system. And like any system, they can be recalibrated-with time, support, and science.
Can anxiety disorders go away on their own?
Sometimes symptoms lessen over time, but they rarely disappear without intervention. Left untreated, anxiety often worsens or leads to other problems like depression, substance use, or avoidance behaviors that limit your life. Early treatment improves long-term outcomes significantly.
Is CBT better than medication?
Neither is universally better. CBT teaches skills that last long after therapy ends. Medication can provide quicker relief and help stabilize mood enough to engage in therapy. For most people, combining both works best. Studies show higher success rates with combined treatment than either alone.
How long does it take for SSRIs to work?
It typically takes 6 to 12 weeks for SSRIs to reach full effect. Some people notice small improvements in sleep or energy after 2-3 weeks, but full symptom reduction takes longer. Patience is key. Don’t stop taking them just because you don’t feel better right away.
Can children have anxiety disorders?
Yes. Half of all anxiety disorders begin by age 11. Children may show it through tantrums, refusal to go to school, clinginess, or physical complaints like stomachaches. Early intervention with CBT tailored for kids is highly effective and can prevent lifelong struggles.
Are anxiety disorders genetic?
Genetics play a role-you’re more likely to develop anxiety if a close relative has it. But environment matters just as much. Trauma, chronic stress, or early life adversity can trigger anxiety even without a family history. It’s a mix of biology and experience.
What if therapy doesn’t work for me?
It doesn’t mean you’re broken. It means you haven’t found the right fit yet. Different therapists use different approaches. Some specialize in ACT, others in exposure therapy or trauma-focused CBT. Try a different provider. Also, medication adjustments, lifestyle changes, or adding digital tools can make a difference. Persistence matters more than perfection.



Nicki Aries
February 2, 2026 at 00:11Finally, someone laid this out without sugarcoating. I’ve been told to ‘just breathe’ for years-like my panic attacks are a bad habit I can quit. The stats on physical symptoms? Spot on. My heart hits 130 bpm during attacks, and no, I don’t ‘choose’ to feel like I’m dying. This post should be mandatory reading for doctors, family members, and anyone who thinks anxiety is ‘all in your head.’
Bryan Coleman
February 2, 2026 at 14:06CBT worked for me-but only after I found a therapist who didn’t rush exposure. I did 3 weeks of just naming my thoughts before touching a doorknob. Took forever, but it stuck. Also, nOCD’s guided logs saved my sanity. Free trial? Do it. No shame in starting small.
Ishmael brown
February 4, 2026 at 00:40SSRIs turned me into a zombie. Not ‘calm’-just empty. Like my emotions got muted by a faulty speaker. I switched to buspirone. No numbness. No weight gain. Just… quieter panic. Also, why is everyone acting like CBT is the holy grail? What about people who can’t afford 20 sessions? Or live in a state with zero therapists? This post feels like a luxury pamphlet.
Nancy Nino
February 4, 2026 at 03:20How refreshing to see evidence-based content presented without the usual wellness fluff. I appreciate the specificity regarding biotypes and AI prediction models-this is the future of mental health care, not Instagram affirmations. Kudos to the author for citing NAMI and FDA-cleared tools. The only missing piece? Data on long-term relapse rates post-treatment.
Ed Di Cristofaro
February 5, 2026 at 16:06People still take this stuff seriously? You’re telling me we need 12 sessions of talking to fix a chemical imbalance? Just take a pill. Or go outside. Or stop being so damn sensitive. My grandpa fought in Korea and never cried about ‘racing thoughts.’ You’re not broken-you’re weak.
Deep Rank
February 6, 2026 at 05:32OMG I feel this so hard!! I have GAD and OCD and I’m like 30 and still washing hands 50x a day and my mom says I’m just attention seeking and I cry every night and my bf left me because I ‘overthink everything’ and I’m like why can’t people just understand?? Also I tried Zoloft and it made me feel like a robot and now I’m on Lexapro and it’s better but I still feel like a disaster and I don’t know what to do anymore
Aditya Gupta
February 7, 2026 at 08:47Exposure therapy is brutal. But worth it. Started with looking at elevator pics. Then standing near one. Then one floor. Took 3 months. Now I ride them without panic. No magic. Just repetition. You got this.
Nidhi Rajpara
February 8, 2026 at 15:38While the article is scientifically sound, it neglects to address the cultural stigma in non-Western societies, particularly in South Asia, where anxiety is often dismissed as ‘lack of spiritual discipline’ or ‘family karma.’ In India, seeking therapy is still seen as a sign of personal failure. This omission limits the post’s global relevance.
Naomi Walsh
February 8, 2026 at 18:12How quaint. You cite ‘FDA-cleared apps’ like they’re equivalent to real clinical care. Have you read the actual trial data on Wysa? The effect size is negligible compared to face-to-face CBT. And ‘zuranolone’? A glorified steroid with a marketing team. This is what happens when Big Pharma funds mental health discourse. Real treatment requires depth, not apps.
Jaden Green
February 10, 2026 at 10:55I read this whole thing. Took me 45 minutes. And honestly? It’s just… a lot. Too many lists. Too many percentages. Too many acronyms. I get that you want to sound smart, but you’re drowning the message in data. I just wanted to know: ‘What do I do today?’ Not the biotype of my amygdala. Just… what do I do? I’m tired.
Jamie Allan Brown
February 12, 2026 at 04:21To the person who said SSRIs made them feel like a robot-I get it. I was on them for two years. Felt like I was watching my life through a foggy window. But here’s what no one tells you: the numbness fades. And when it did, I finally had space to breathe. I started ACT. Not to fix my thoughts, but to stop fighting them. Now I write poetry about panic attacks. Weird? Maybe. Healing? Absolutely.