Triptans are effective for migraines but come with serious interactions and limitations. Learn who should avoid them, why they sometimes fail, and what to do when they don't work.
Triptan Side Effects: What You Need to Know Before Taking Migraine Medication
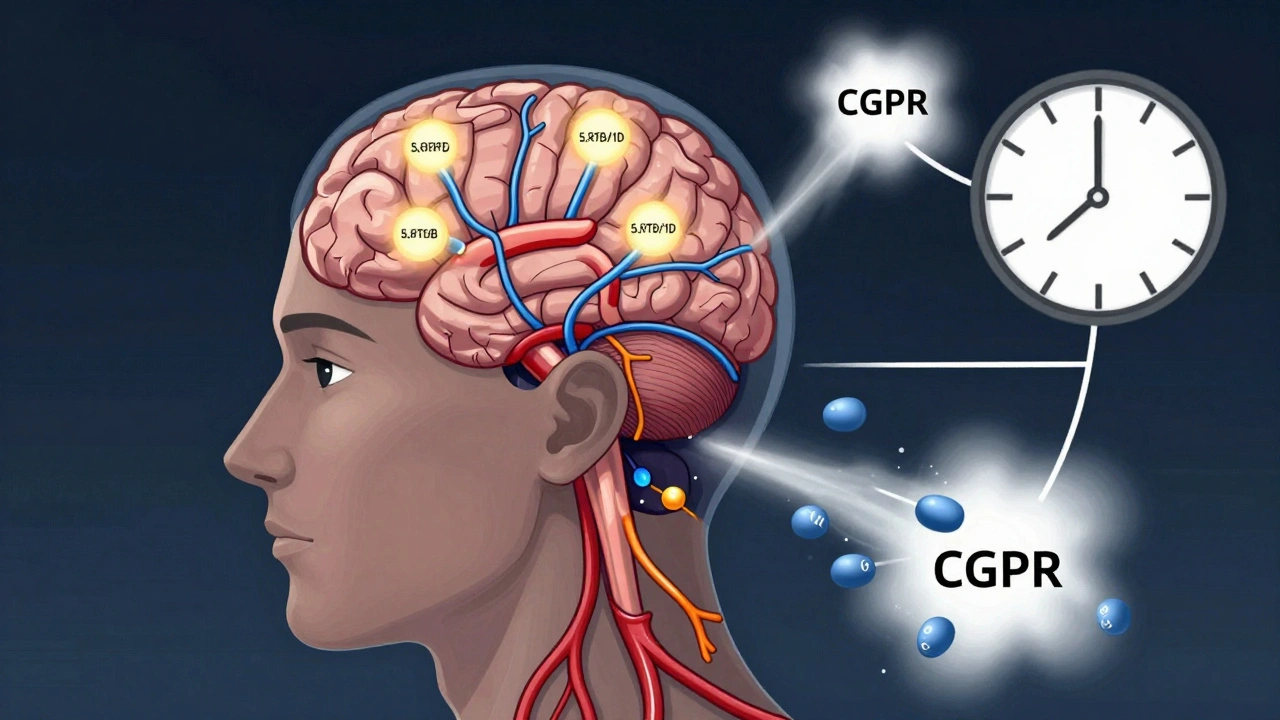
When you’re in the middle of a migraine, triptans, a class of prescription drugs designed to stop migraine attacks by narrowing blood vessels in the brain and blocking pain pathways. Also known as serotonin receptor agonists, they’re one of the most effective tools for acute migraine relief. But like all powerful medications, they come with risks—some mild, some serious—that you need to understand before taking them. Many people assume triptans are harmless because they work so well, but side effects aren’t just annoying—they can be dangerous if ignored.
Common triptan side effects include nausea, dizziness, fatigue, and a feeling of tightness in the chest, throat, or limbs. These usually fade quickly and aren’t life-threatening. But some reactions—like sudden chest pain, shortness of breath, or unusual heart rhythms—can signal something worse. Triptans can trigger serious cardiovascular events in people with untreated high blood pressure, heart disease, or a history of stroke. If you’re over 40, smoke, or have diabetes, your doctor should check your heart health before prescribing them. And never take triptans with certain antidepressants like SSRIs or SNRIs. That combo can cause serotonin syndrome, a rare but deadly condition where your body makes too much serotonin, leading to high fever, seizures, or irregular heartbeat.
Another hidden risk is medication-overuse headache. If you take triptans more than 10 days a month, you might start getting headaches more often—not less. It’s not your migraine getting worse; it’s the medicine itself causing the problem. This is why doctors limit prescriptions and push for prevention strategies alongside acute treatment. You also need to know that not all triptans are the same. Sumatriptan, rizatriptan, eletriptan—they differ in how fast they work, how long they last, and what side effects they cause. One might give you a tight chest; another might make you sleepy. Finding the right one takes trial and careful tracking.
What’s missing from most patient conversations is the role of lifestyle and other medications. If you’re on blood pressure pills, birth control, or even over-the-counter painkillers like NSAIDs, those can change how triptans behave in your body. And if you’re using them for tension headaches or cluster headaches—off-label uses—you’re increasing your risk without guaranteed benefit. The FDA has warned about rare cases of stroke and heart attack linked to triptans, especially when used incorrectly.
Below, you’ll find real-world insights from patients and clinicians on how triptans actually perform in daily life—not just in clinical trials. You’ll learn how to spot warning signs early, how to talk to your pharmacist about interactions, and what alternatives exist when triptans don’t work—or when they’re too risky. These aren’t theoretical discussions. They’re based on reports from people who’ve been there, and the data that backs them up.