Step therapy forces patients to try cheaper generic drugs before insurers cover more expensive treatments. Learn how it works, when it fails, and what you can do to get exceptions quickly.
Step Therapy: What It Is, Why It’s Used, and How It Affects Your Medication Access
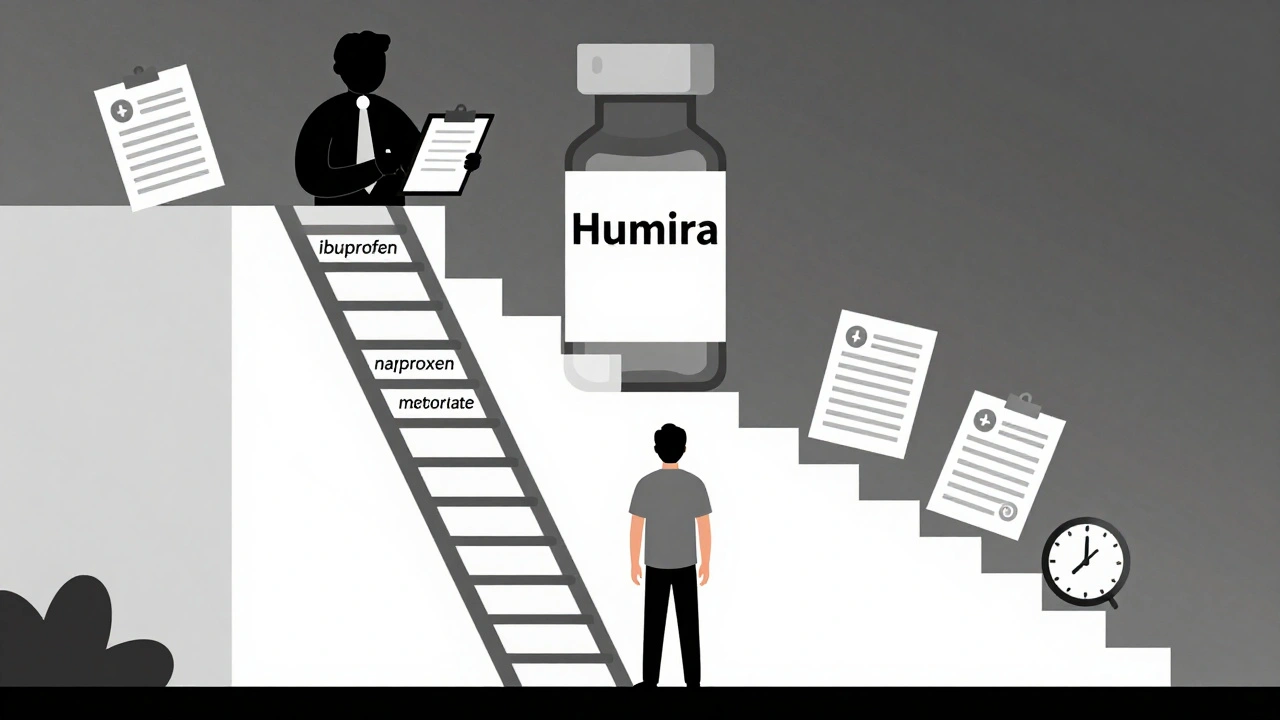
When your insurance won’t cover the drug your doctor ordered right away, you’re likely facing step therapy, a requirement that you try one or more lower-cost medications before getting approval for the prescribed treatment. Also known as fail first, it’s a common tool used by health plans to control spending—but it doesn’t always match what’s best for your health. This isn’t about being cheap. It’s about following a protocol: if a generic statin or a basic blood pressure pill can do the job, insurers want you to try it first—even if your doctor thinks a different drug would work better, faster, or with fewer side effects.
Step therapy is tied closely to prior authorization, a process where insurers review and approve certain prescriptions before filling them. These two systems often work together. Your pharmacy might hold your prescription until your doctor submits paperwork proving you’ve tried—and failed—the cheaper options. That delay can mean weeks without proper treatment, especially for chronic conditions like arthritis, depression, or diabetes. And while insurers claim step therapy improves outcomes by avoiding expensive drugs unless necessary, real-world data shows it often leads to more hospital visits, increased pain, and dropped prescriptions altogether.
It’s not just about price. medication access, the ability to get the right drug at the right time without unnecessary barriers is at stake. Many patients end up switching to drugs they tolerate poorly, or give up entirely because the paperwork is too much. The system assumes all patients respond the same way to medications—but we know that’s not true. One person’s safe, effective generic might be another’s nightmare of side effects. That’s why doctors push back: step therapy often ignores individual biology, medical history, and treatment goals.
What you’ll find in the posts below isn’t just theory. These are real stories and facts from people who’ve fought insurance denials, worked with pharmacists to bypass step therapy hurdles, and learned how to navigate the maze of insurance requirements, the rules health plans use to limit drug choices and control costs. You’ll see how drug coverage, what your plan actually pays for, and what it blocks changes depending on where you live, what plan you have, and even which pharmacy you use. Some posts break down how hospitals and pharmacies push back against step therapy. Others show you how to appeal a denial or get your doctor to write a strong letter of medical necessity. This isn’t about fighting the system—it’s about understanding it well enough to work within it without sacrificing your health.