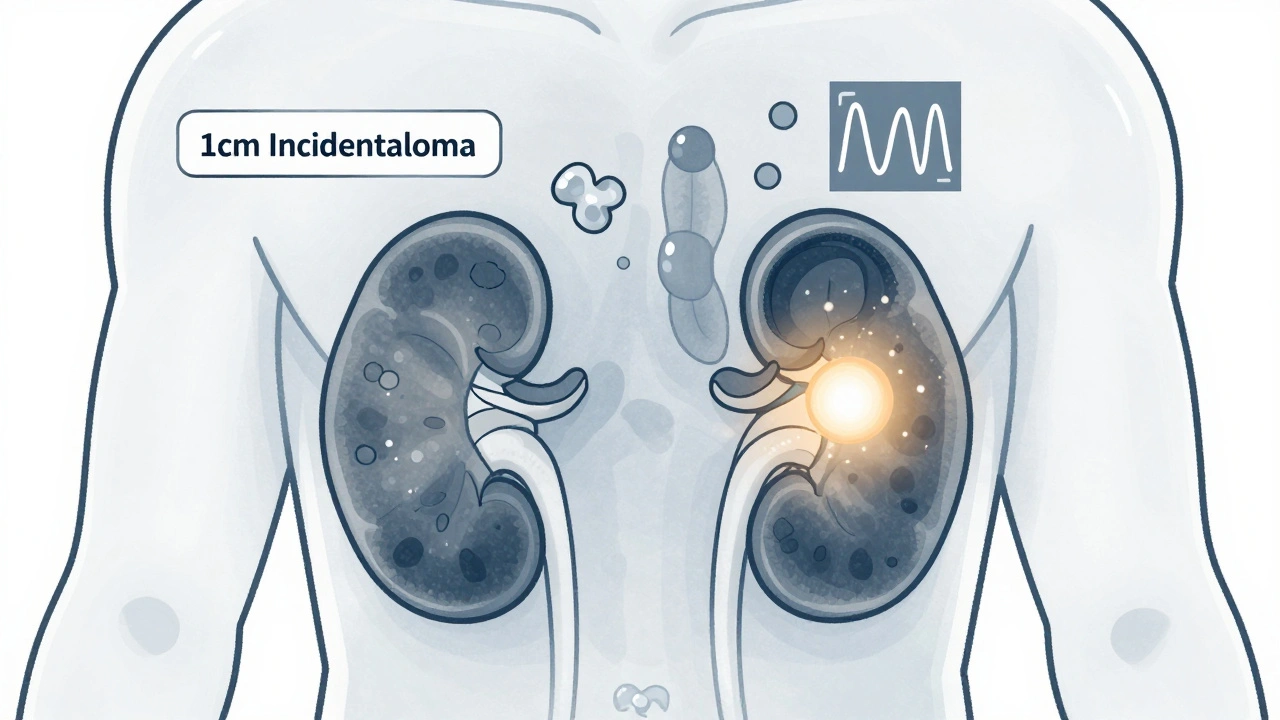
Adrenal incidentalomas are common findings on imaging scans. Most are harmless, but some can cause serious health problems. Learn how to tell the difference and when surgery is truly needed.
Pheochromocytoma: Symptoms, Diagnosis, and Treatment Options
When your body releases too much catecholamines, hormones like adrenaline and noradrenaline that control heart rate, blood pressure, and stress response, things can go wrong fast. That’s what happens with pheochromocytoma, a rare, usually noncancerous tumor that grows on the adrenal glands and overproduces these hormones. It’s not common—only about 2 to 8 cases per million people each year—but when it shows up, it doesn’t whisper. It screams with pounding headaches, sweating so heavy it soaks your clothes, and blood pressure spikes that can land you in the ER thinking it’s a heart attack.
Pheochromocytoma is a type of adrenal tumor, a growth on the adrenal glands located just above the kidneys, and it’s often missed because its symptoms look like anxiety, panic attacks, or even menopause. But unlike those conditions, the episodes come in waves—sudden, intense, and unpredictable. You might feel your heart racing for no reason, your vision blurring, or your hands trembling while sitting quietly. These aren’t just stress reactions. They’re chemical storms triggered by the tumor releasing bursts of adrenaline into your bloodstream. Left untreated, these surges can cause strokes, heart failure, or even sudden death.
Diagnosis starts with blood or urine tests that measure catecholamine levels during an episode. If those are high, imaging like a CT or MRI scans the adrenal glands to find the tumor. In some cases, genetic testing is needed because pheochromocytoma can run in families linked to conditions like neurofibromatosis or MEN2 syndrome. Treatment almost always means surgery to remove the tumor, but it’s not as simple as just cutting it out. Doctors have to carefully control blood pressure for days before the operation using medications like alpha-blockers. Skip that step, and the stress of surgery could trigger a fatal surge.
After surgery, most people recover fully—but monitoring continues. In about 10% of cases, the tumor comes back, or a second one develops elsewhere. That’s why follow-up blood tests and scans are part of the long-term plan. And while surgery is the main fix, knowing what triggers an episode helps you avoid them: caffeine, intense stress, certain medications like decongestants, and even bowel movements can set off a crisis. This isn’t just about managing a tumor. It’s about learning how to live safely with a hidden time bomb in your body.
Below, you’ll find real-world guides on how insurance handles rare disease treatments, why generic drug quality matters when you’re on long-term meds, and how patient counseling can catch errors before they hurt you. These aren’t abstract topics—they’re the practical tools you need when dealing with something as unpredictable as pheochromocytoma.