HRT Risk & Benefit Calculator
Assess Your Personalized HRT Risk
Based on your age, menopause timing, and health history, this tool estimates your relative risk of side effects compared to the general population.
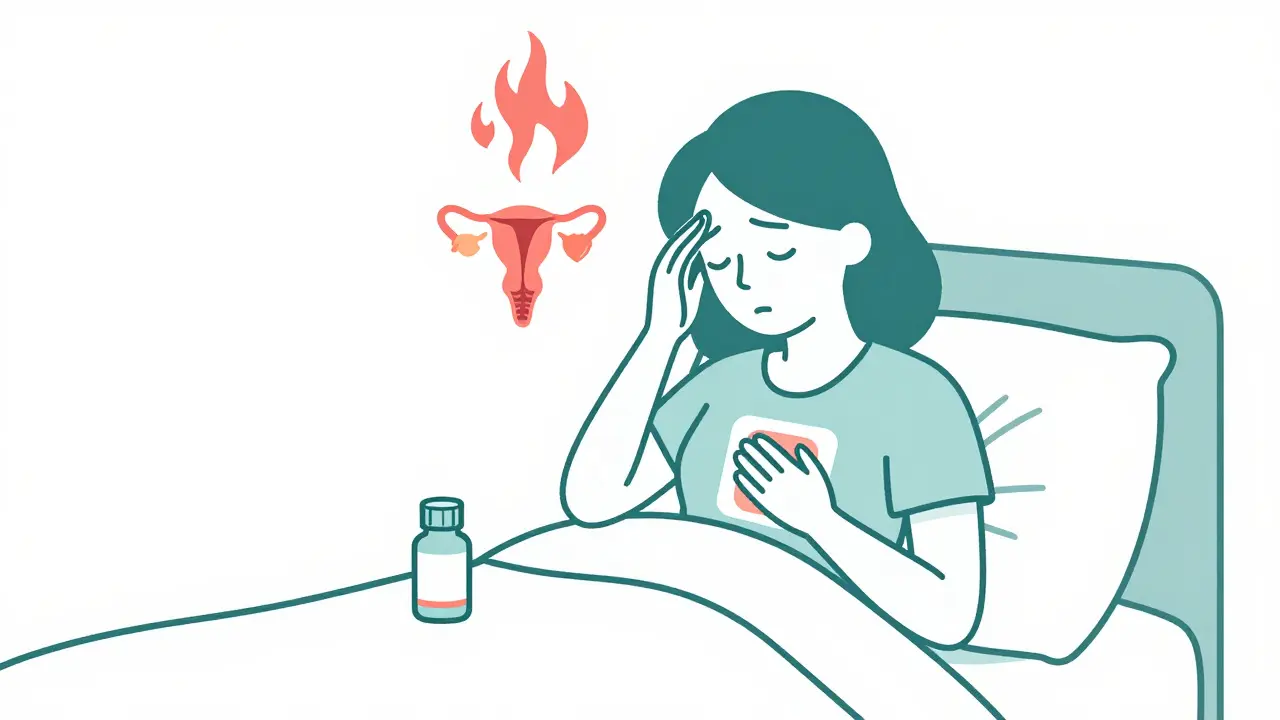
When menopause hits, your body doesn’t just slow down-it rewires itself. Hot flashes wake you up at 3 a.m. Vaginal dryness makes sex painful. Mood swings turn small frustrations into big explosions. For many women, these aren’t just inconveniences-they’re life disruptors. That’s why millions turn to hormone therapy. But here’s the thing: what helps one woman might hurt another. The side effects of menopause medications aren’t one-size-fits-all. They change based on your age, your health history, and even how you take the pill-or patch-or gel.
What Hormone Therapy Actually Does
Menopause hormone therapy (HRT) replaces the estrogen and sometimes progesterone your ovaries stop making. That’s it. No magic. No miracle. Just chemistry trying to balance what your body used to handle on its own. Estrogen alone works for women who’ve had a hysterectomy. If you still have a uterus, you need progesterone too-otherwise, you risk endometrial cancer. That’s why combination therapy exists.
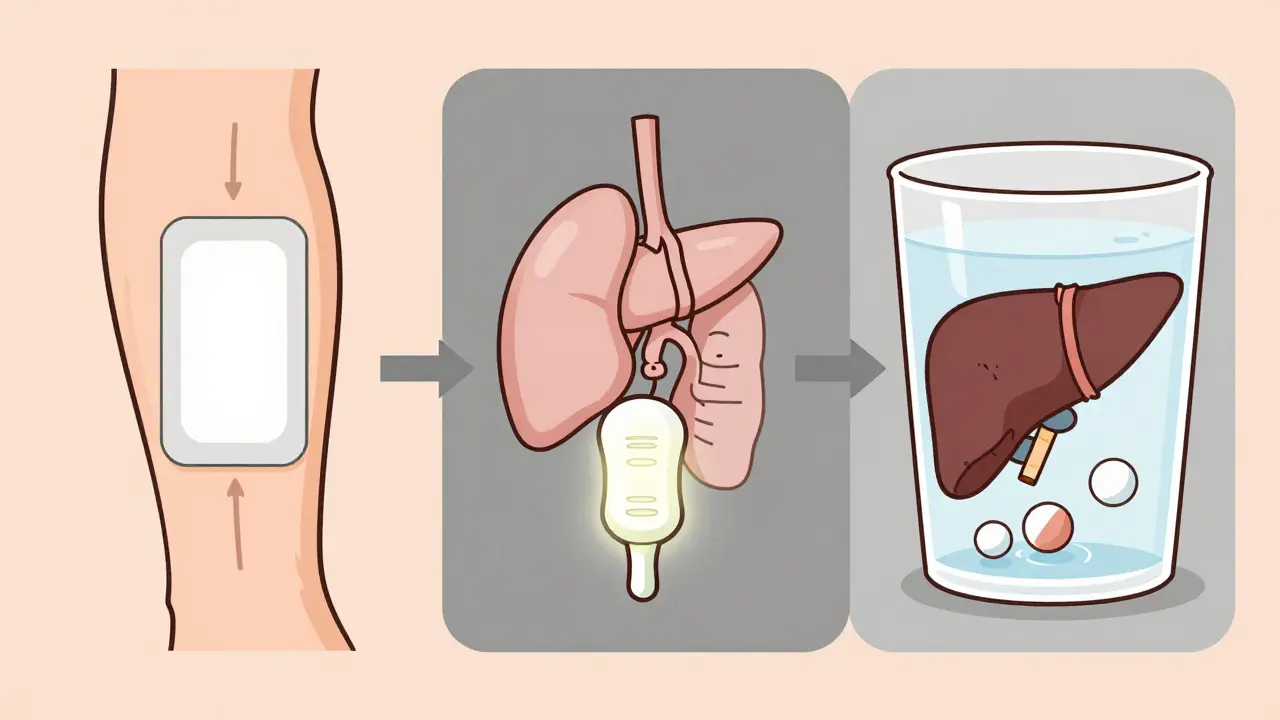
The FDA approves several forms: pills like Duavee (conjugated estrogen + bazedoxifene), patches you stick on your skin, gels you rub on your arms, creams for vaginal use, and even tiny inserts that dissolve inside the vagina. Each has different absorption rates, different side effect profiles, and different risks. A patch doesn’t hit your liver the same way a pill does. That matters.
The Real Risks You Can’t Ignore
Let’s cut through the noise. Yes, HRT can increase your risk of certain serious problems. But numbers don’t scare people-context does.
According to the Women’s Health Initiative study, combination HRT raises the chance of breast cancer by 26% over five years. Sounds scary? Let’s put it in perspective: for every 10,000 women taking it, the number of breast cancer cases goes from 30 to 38. That’s 8 extra cases. For stroke? It jumps from 21 to 29 cases per 10,000. Blood clots? A 113% increase in lung clots-but that’s still only 3 to 7 cases per 10,000 women each year.
Age is the biggest factor. If you start HRT before 60 or within 10 years of your last period, your heart risk is lower. Start later? Your chance of heart attack or stroke rises by 24%. That’s why doctors now talk about the “window of opportunity.” It’s not about avoiding HRT entirely-it’s about timing it right.
And then there’s dementia. Women 65 and older on HRT have more than double the risk of developing it. That’s why most guidelines say: don’t use it for brain protection. Use it for symptoms. Period.
Common Side Effects-and What to Do About Them
Most side effects aren’t life-threatening. They’re annoying. And most fade.
- Spotting or bleeding: 30-50% of women get this in the first 3-6 months. It’s normal. If it keeps going past six months? Call your doctor. It could mean your dose is off.
- Breast tenderness: 20-40% of users feel it. Often goes away in a few weeks. If it’s painful or one-sided, get it checked.
- Bloating and fluid retention: Affects 15-25%. Switching from pills to patches cuts this by 60%.
- Headaches: 10-25% of users. Often tied to estrogen levels. Lowering the dose helps.
- Mood changes: 20-25% report irritability or low mood. For some, estrogen helps. For others, it makes it worse. If you’re prone to depression, talk to your doctor before starting.
Here’s what works: give it three months. Most side effects settle down. If they don’t, don’t suffer. Your doctor can adjust your dose, switch the type (like from oral to patch), or try a different delivery method. One study found 68% of women found relief just by tweaking the dose.
Alternatives That Actually Work
You don’t need hormones to feel better. Many women choose non-hormonal options-and they work.
- SSRIs like escitalopram or paroxetine: Reduce hot flashes by 50-60% in 60% of users. No estrogen. No breast cancer risk.
- Gabapentin: A nerve pain drug that cuts hot flashes by 45%. Good for women who can’t take hormones.
- Clonidine: An old blood pressure pill that reduces hot flashes by 46%. Can cause dry mouth or dizziness.
- Vaginal DHEA (Intrarosa): A tiny insert that improves sexual pain in 70% of users. Minimal absorption into the bloodstream.
- Vaginal moisturizers and lubricants: Used by 45% of menopausal women. Simple, safe, and effective for dryness.
And yes, black cohosh? Mixed results. 12 studies. 1,845 women. No clear winner. Avoid anything labeled “natural” unless it’s been tested in real trials.
What’s New on the Horizon
The field is changing fast. In 2024, the FDA is expected to approve fezolinetant-a new drug that blocks a brain signal causing hot flashes. In trials, it cut moderate-to-severe hot flashes by over 50%. No hormones. No breast cancer risk. Just science.
Low-dose vaginal estrogen is also getting smarter. New formulations release less into the bloodstream, making them safer for long-term use. And tissue-selective estrogen complexes? They act like estrogen in bones and skin, but not in breast or uterine tissue. That’s the future: precision, not blanket treatment.

How to Decide What’s Right for You
There’s no perfect answer. Only the right one-for you.
Ask yourself:
- How bad are my symptoms? If I can’t sleep, work, or have sex, is the risk worth the relief?
- What’s my health history? Any blood clots, breast cancer, stroke, or liver disease? Then HRT is likely off the table.
- How old am I? Am I within 10 years of menopause? If yes, the benefits usually outweigh the risks.
- Am I willing to try non-hormonal options first? Many women find relief without hormones.
Start low. Go slow. Use the lowest dose that works. Choose the patch or gel if you can. Avoid pills if you have a history of clots. And never start HRT just to prevent osteoporosis-there are safer drugs for that.
What to Do If Side Effects Stick Around
If you’ve been on HRT for three months and you’re still feeling off, don’t just quit. Talk to your doctor. Here’s what they might suggest:
- Change the dose: Lowering estrogen often cuts side effects without losing symptom control.
- Switch delivery: Patches avoid the liver, so they’re gentler on your stomach and blood clot risk.
- Try a different progestin: Some cause less bloating or mood swings than others.
- Add a non-hormonal boost: Gabapentin for hot flashes, SSRIs for mood-combined therapy can reduce hormone dose.
And if you miss a pill? Don’t double up. Take it when you remember. If it’s almost time for the next one, skip it. Double doses raise side effect risks.
Final Thought: It’s Not About Fear. It’s About Fit.
Menopause isn’t a disease. But the symptoms can feel like one. Hormone therapy isn’t a cure. But for many women, it’s the best tool they’ve got.
The goal isn’t to avoid all risk. It’s to pick the right level of risk for your life. If hot flashes keep you awake every night, and you’re healthy and under 60, HRT might be the answer. If you’re 65, have a family history of breast cancer, and just want to stop night sweats? There are other options.
Your body changed. Your treatment should too. Don’t let outdated fears stop you. Don’t let marketing push you. Talk to your doctor. Test the options. Adjust. Reassess. Menopause lasts decades. Your treatment should too.
Is hormone replacement therapy safe for menopause?
For healthy women under 60 or within 10 years of menopause, HRT is generally safe for symptom relief. The risks-like blood clots, stroke, and breast cancer-are low for most but increase with age, longer use, and certain health conditions. It’s not for everyone, but for many, the benefits outweigh the risks when used correctly.
What are the most common side effects of HRT?
The most common side effects include vaginal spotting (30-50% of users), breast tenderness (20-40%), bloating (15-25%), headaches (10-25%), and mood changes (20-25%). Most improve within 3-6 months. If they don’t, your dose or delivery method may need adjusting.
Can I take HRT if I’ve had breast cancer?
No. Hormone replacement therapy is not recommended for women with a history of breast cancer, endometrial cancer, or any estrogen-sensitive cancer. Even low-dose or local estrogen can stimulate cancer cells. Non-hormonal options like SSRIs, gabapentin, or vaginal DHEA are safer alternatives.
Are patches safer than pills for HRT?
Yes. Transdermal patches and gels deliver estrogen through the skin, bypassing the liver. This lowers the risk of blood clots by 30-40% compared to oral pills. They’re also easier on the stomach and cause less bloating. For women with a history of clots or liver issues, patches are often the preferred choice.
How long should I stay on hormone therapy?
There’s no fixed timeline. Most women use HRT for 2-5 years to manage symptoms. Some need it longer, especially if symptoms persist after 60. The key is using the lowest effective dose for the shortest time needed. Reassess annually with your doctor. Don’t stay on it just because you started.
What are the best non-hormonal treatments for hot flashes?
The most effective non-hormonal options are SSRIs (like paroxetine), gabapentin, and clonidine. SSRIs reduce hot flashes by 50-60% in 60% of users. Gabapentin cuts them by 45%. Clonidine works for about half of users. Vaginal moisturizers help with dryness, and low-dose vaginal DHEA (Intrarosa) improves sexual pain in 70% of women.
Can herbal supplements like black cohosh help with menopause symptoms?
Studies on black cohosh show mixed results. Twelve clinical trials involving over 1,800 women found no consistent benefit over placebo. Other herbs like red clover or dong quai haven’t been proven safe or effective. The FDA doesn’t regulate supplements, so quality and ingredients vary. Stick with evidence-based treatments unless your doctor approves a trial.
When should I stop HRT?
You should consider stopping HRT if your symptoms improve, you’ve been on it for more than 5 years, or if you develop new health risks like high blood pressure, blood clots, or abnormal breast changes. Annual check-ins with your doctor help determine if you still need it. Never stop suddenly-tapering reduces rebound symptoms.

Dusty Weeks
December 31, 2025 at 22:26I swear if one more person says "just take hormones" I'm gonna scream 😤 My aunt got breast cancer after 2 years on HRT and now she's gone. They make it sound like it's just a cold, but it's not. Don't be that person.
Sally Denham-Vaughan
January 1, 2026 at 14:43Honestly? I tried the patch, hated the bloating, switched to gel, and now I’m sleeping through the night for the first time in 3 years. No drama. No guilt. Just me and my cool skin lotion. 🙌
Bill Medley
January 2, 2026 at 23:33The data is clear. Risk-benefit analysis must be individualized. Age at initiation and route of administration are primary determinants of safety.
Richard Thomas
January 4, 2026 at 05:46It’s funny how we treat menopause like a medical emergency instead of a natural transition. We’ve spent decades pathologizing women’s bodies while ignoring the social and psychological weight of aging. The real side effect isn’t the hormone-it’s the expectation that we should be able to stay young forever. Maybe the problem isn’t our biology, but our culture’s refusal to let go.
Paul Ong
January 6, 2026 at 03:44Patch over pill any day if you got clots in your family or just hate feeling like a balloon. Also gabapentin actually worked for me like a charm no mood swings just chill
Andy Heinlein
January 7, 2026 at 16:09Y’all are overthinking this. I started low dose patch, gave it 3 months, and now I’m hiking again. No drama. No guilt. Just me being me. If it ain’t broke don’t fix it but if it is fix it smart
Ann Romine
January 7, 2026 at 20:59In my culture, menopause is spoken of in hushed tones, if at all. It’s seen as a loss of power. But reading this made me realize it’s not the end-it’s a shift. I’m going to share this with my mother. She’s been suffering in silence for years.
Todd Nickel
January 8, 2026 at 11:07The assumption that all women experience menopause the same way is dangerously reductive. The pharmacokinetics of transdermal estrogen versus oral formulations aren’t just academic-they’re life-altering. The liver’s first-pass metabolism significantly elevates clotting factors, which is why patch users have lower VTE risk. This isn’t opinion; it’s clinical pharmacology. Yet most primary care providers still default to pills because they’re cheaper and easier to prescribe. We need better education-not just for patients, but for practitioners.
Austin Mac-Anabraba
January 9, 2026 at 11:43Let’s be real. Big Pharma pushed HRT for decades like it was a fountain of youth. Now they’re quietly backing away because the lawsuits are piling up. You think they care about your hot flashes? They care about your insurance billing codes. Read the fine print. The ‘window of opportunity’? That’s just a marketing slogan wrapped in science-speak.
Phoebe McKenzie
January 10, 2026 at 14:27I can’t believe people still fall for this. Hormones are poison. They turn your body into a cancer factory. I’ve seen women turn into monsters on HRT-angry, bloated, emotional wrecks. It’s not menopause, it’s chemical madness. And now they want to give it to teens? Next they’ll be giving estrogen to boys to ‘help them feel better.’ Wake up people. This isn’t medicine. It’s control.
gerard najera
January 12, 2026 at 03:56Patches reduce liver exposure. That’s it.
Stephen Gikuma
January 13, 2026 at 21:58They’re slipping estrogen into our water. You think this is about menopause? It’s about population control. Look at the stats-women who take HRT are more likely to die. Coincidence? Or is this the elite’s way of thinning the herd? Don’t drink the Kool-Aid.
LIZETH DE PACHECO
January 14, 2026 at 23:51I was scared to even ask my doctor about this. But after reading this, I made an appointment. We switched me from pills to gel and my mood is finally stable. Thank you for writing this. I didn’t feel alone anymore.
Lee M
January 15, 2026 at 19:40The real issue isn’t HRT. It’s that we’ve turned menopause into a problem to be fixed instead of a phase to be understood. Women aren’t broken. The system is.