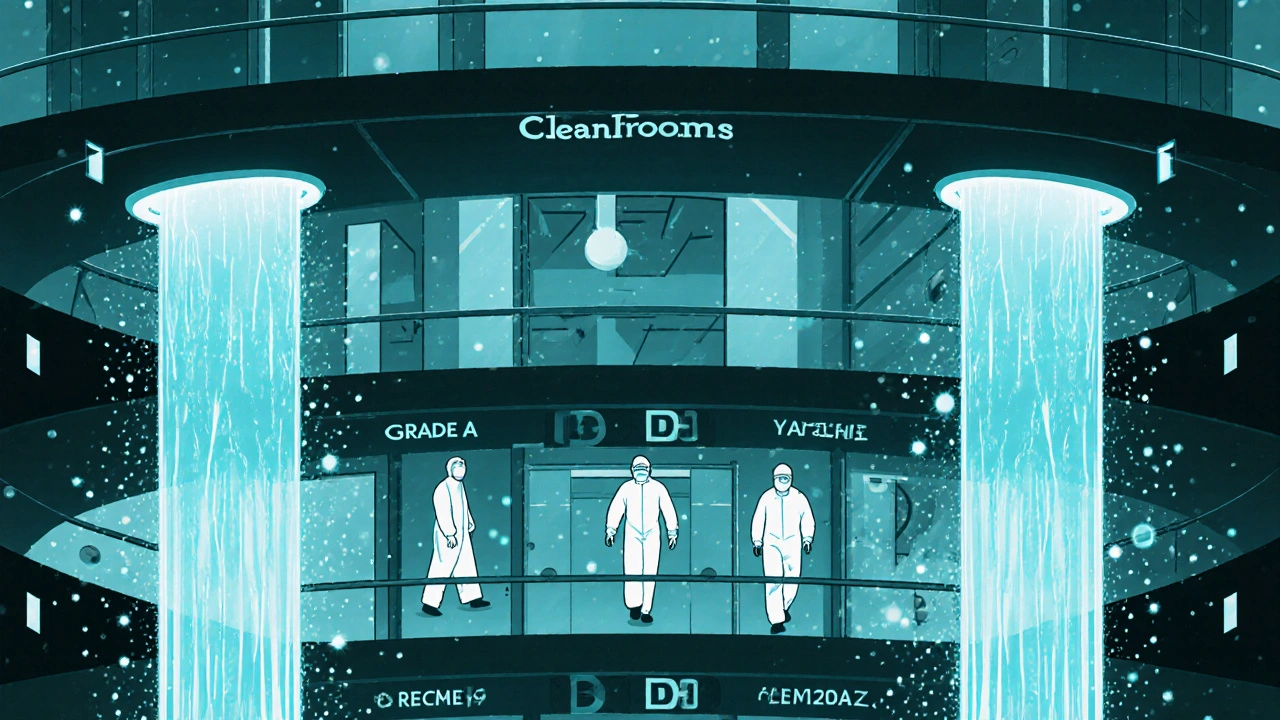
Cleanroom standards ensure generic drugs are safe and effective by controlling airborne particles, microbes, and environmental conditions. Learn how ISO grades, FDA/EU rules, and human factors impact quality - and why compliance isn't optional.
Generic Drug Quality: What You Need to Know About Safety, Effectiveness, and Regulation
When you pick up a generic drug, a medication that contains the same active ingredient as a brand-name drug but is sold under its chemical name. Also known as non-brand medication, it is designed to work the same way, at the same dose, and with the same safety profile as the original. But here’s the catch: not all generics are made the same. The FDA says they’re equivalent — and for most people, they are. But behind that label are differences in inactive ingredients, manufacturing processes, and even the source of the active drug. These aren’t just technical details. They can affect how a pill dissolves, how your body absorbs it, and whether it causes unexpected side effects.
That’s where pharmaceutical quality, the set of standards ensuring a drug is safe, effective, and consistently produced. Also known as drug manufacturing standards, it determines whether a generic pill works the same batch after batch. Hospitals don’t just pick generics because they’re cheap. They look at reliability, supply chain stability, and how often a batch gets flagged for impurities. One hospital switch from one generic version of a blood thinner to another led to a spike in clotting events — not because the active ingredient changed, but because the coating and fillers affected how fast it released into the bloodstream. This isn’t rare. It’s why the FDA requirements, the rules set by the U.S. Food and Drug Administration to ensure drug safety and consistency. Also known as regulatory standards for pharmaceuticals, it governs everything from how a tablet is pressed to how a factory is inspected. matter so much. And it’s why some doctors avoid switching patients between different generic brands unless absolutely necessary.
Then there’s the gray area: biosimilars, highly similar versions of complex biologic drugs that can’t be copied exactly like traditional pills. Also known as follow-on biologics, they’re not generics, but they’re often grouped with them — and that’s where confusion starts. Biologics like Humira or Enbrel are made from living cells, not chemicals. Even tiny changes in the production process can alter how they work. That’s why biosimilars require years of testing and why they’re not interchangeable by default. But in many places, pharmacies still substitute them without telling you. You might think you’re getting the same thing — but the science says otherwise.
What you’ll find in these articles isn’t marketing fluff or vague warnings. It’s real talk from people who’ve seen the fallout: a patient whose blood pressure spiked after a generic switch, a hospital pharmacist who had to explain why two "identical" pills behaved differently, a doctor who learned the hard way that federal preemption laws leave them exposed when a generic causes harm. You’ll read about how manufacturing changes are approved — or ignored — and why some generics pass inspection but still cause problems. You’ll learn how formularies choose which generic to stock, and why price isn’t always the deciding factor. This isn’t about fearing generics. It’s about understanding what makes one better than another — and how to protect yourself.