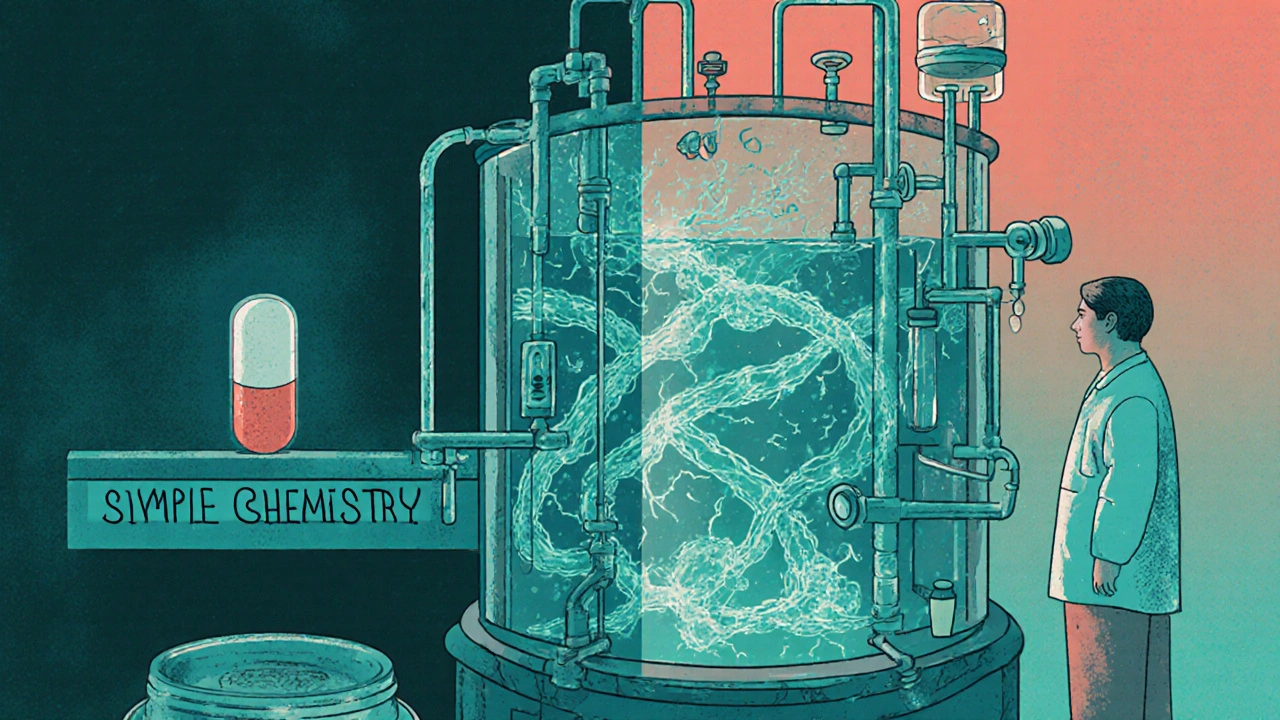
Biologic drugs are made from living cells, not chemicals, making them impossible to copy exactly. That’s why biosimilars aren’t generics - they’re highly similar versions that still require complex manufacturing and rigorous testing.
Complex Medicines: What They Are, Why They Matter, and What You Need to Know
When we talk about complex medicines, pharmaceutical products with intricate chemical structures, multiple active ingredients, or advanced delivery systems that require strict manufacturing control. Also known as highly specialized drugs, they include biologics, combination therapies, and modified-release formulations that can’t be easily copied or substituted. These aren’t your standard aspirin or antibiotic. They’re the kind of drugs that need factory-level precision to make safely—and even then, small changes can change how they work in your body.
That’s why manufacturing changes, any adjustment in how a complex medicine is produced, from raw materials to packaging. Also known as change control, it’s not just paperwork—it’s a legal and safety requirement. A single tweak in temperature during production, or switching a supplier for an inactive ingredient, can alter how the drug dissolves in your gut. The FDA and other global regulators demand notification and approval for these changes because they directly affect pharmaceutical quality, the consistency, purity, and effectiveness of a drug from batch to batch. Also known as drug integrity, it’s what keeps you safe when you take the same pill week after week. One wrong move, and you could get a version that doesn’t work—or worse, causes harm.
And it’s not just about making the drug right. drug interactions, when two or more medicines react in your body in unexpected ways. Also known as medication conflicts, they’re especially dangerous with complex medicines. Take gabapentinoids and opioids together? You risk breathing problems—even at normal doses. Mixing statins with certain antibiotics? That could trigger heart rhythm issues. These aren’t rare edge cases. They’re documented, preventable risks that show up in real patient reports to the FDA. And when hospitals switch generic versions of these drugs, they’re not just saving money—they’re playing Russian roulette with clinical outcomes. Formularies don’t always tell you why they made the switch, and patients rarely know they’re on a different version of the same pill.
What makes complex medicines even trickier is that they often treat serious, long-term conditions—like osteoporosis, Parkinson’s, hepatitis C, or low testosterone. That means people take them for years. Small differences in how they’re made, absorbed, or metabolized can add up. That’s why knowing the difference between brand and generic isn’t just about cost. It’s about control. It’s about understanding that not all pills with the same name are the same. And it’s why reporting side effects matters. Your report to MedWatch might help catch a pattern no one else saw.
Below, you’ll find real-world breakdowns of how these medicines work, what can go wrong, and how to protect yourself. From how a change in manufacturing can affect your bone density drug to why your heart rhythm might be at risk from a simple antibiotic, these posts give you the facts—not the marketing. You’re not just taking a pill. You’re managing a system. And you deserve to know how it all fits together.