Cleanroom standards ensure generic drugs are safe and effective by controlling airborne particles, microbes, and environmental conditions. Learn how ISO grades, FDA/EU rules, and human factors impact quality - and why compliance isn't optional.
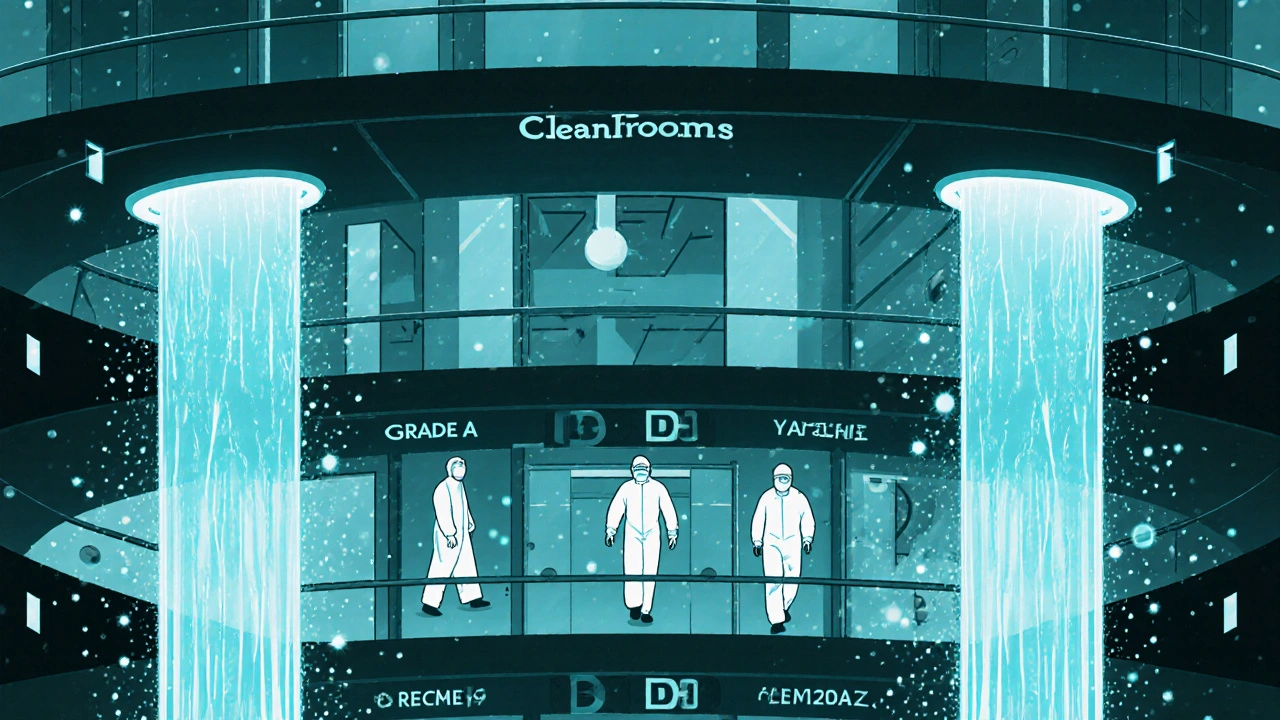
Cleanroom Standards: What You Need to Know About Pharmaceutical Cleanroom Requirements
When you take a pill, you expect it to be pure, safe, and exactly as it should be. That’s not luck—it’s the result of cleanroom standards, controlled environments designed to minimize airborne particles and microbial contamination in pharmaceutical manufacturing. Also known as GMP cleanroom, these spaces are where medicines are made under strict rules that leave no room for error. One wrong move—a sneeze, a loose thread, a poorly sealed door—and you could contaminate an entire batch of life-saving drugs. That’s why cleanroom standards aren’t just guidelines; they’re the backbone of drug safety.
These standards are built around ISO 14644, an international system that classifies cleanrooms by how many particles are allowed per cubic meter of air. This isn’t theoretical—it’s measured in real time with sensors that count dust, skin flakes, and microbes. A Class 7 cleanroom, common in pharma, allows no more than 352,000 particles of 0.5 microns or larger. Compare that to a typical office, which can have over 10 million. And it’s not just about air. Workers wear full gowns, gloves, masks, and shoe covers. Surfaces are wiped down hourly. Even the air is filtered through HEPA systems that trap 99.97% of particles. All of this ties directly to contamination control, the practice of preventing foreign substances from entering drugs during production. Without it, you risk infections, allergic reactions, or even fatal outcomes.
Regulators like the FDA and EMA don’t just check paperwork—they send inspectors to walk through cleanrooms, watch procedures, and test surfaces. If you’re working in pharma, you know that a single violation can shut down production for weeks. That’s why companies train staff for months, not days. They use automated systems to track who enters, when, and what they did. They monitor temperature, humidity, and pressure differences between rooms to keep contaminants from creeping in. And every change—from new equipment to a different cleaning agent—must be documented and approved. This isn’t just about compliance. It’s about trust. Patients trust that their medicine won’t make them sicker. Cleanroom standards make that trust possible.
What you’ll find below are real-world examples of how these rules play out: how manufacturing changes are reported, why biologic drugs need even tighter controls, how formularies rely on clean production, and how even small mistakes can lead to recalls. These aren’t abstract rules—they’re the quiet, invisible systems keeping millions of people safe every day.