Ankylosing spondylitis causes chronic spine inflammation and stiffness. TNF inhibitors like Humira and Enbrel target the root cause, reducing pain, improving mobility, and slowing disease progression for many patients.
Biologic Drugs: What They Are, How They Work, and What You Need to Know
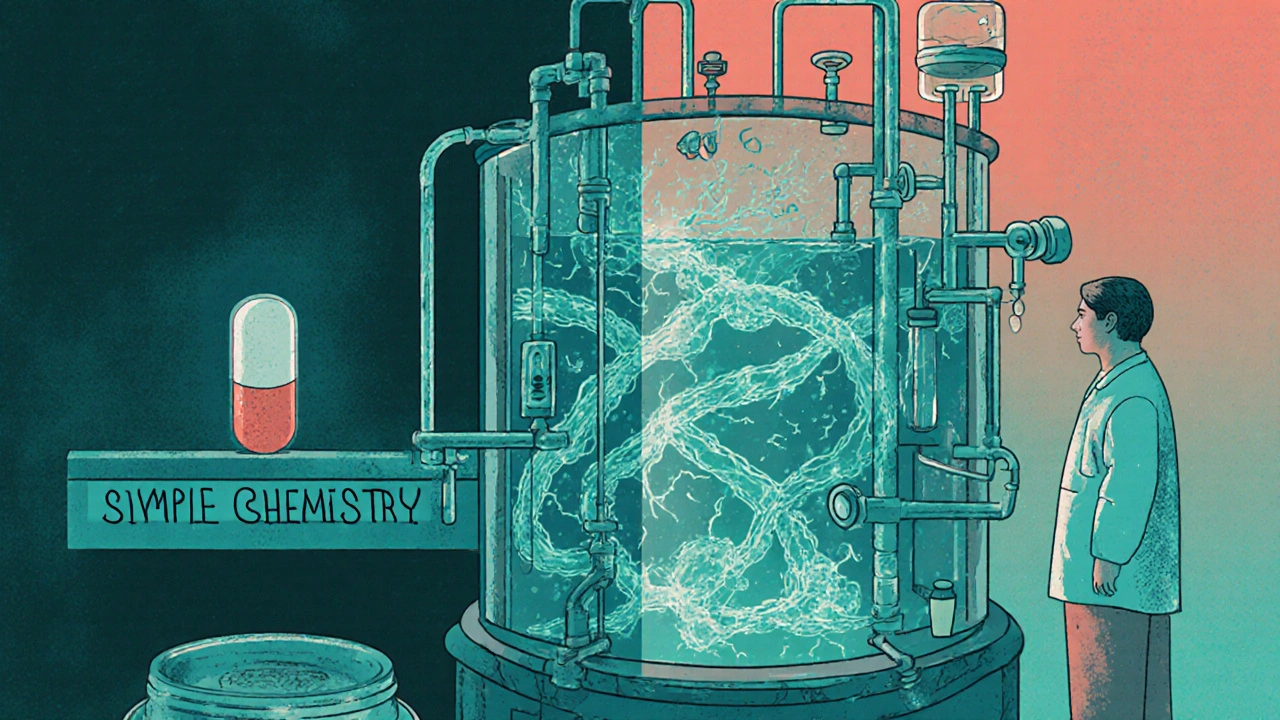
When you hear biologic drugs, complex medicines made from living cells, not chemicals, used to treat serious diseases like rheumatoid arthritis, Crohn’s disease, and certain cancers. Also known as biopharmaceuticals, they are not the same as traditional pills. These drugs are grown in living systems—like yeast, bacteria, or animal cells—and are far more intricate than synthetic compounds. Because of their size and structure, they can’t be copied exactly, which is why similar versions are called biosimilars, drugs that are highly similar to an original biologic but not identical, approved after rigorous testing for safety and effectiveness.
Biologic drugs work by targeting specific parts of the immune system or disease process. For example, some block proteins that cause inflammation, while others train your body’s immune cells to attack cancer. This precision makes them powerful, but also expensive and sometimes risky. They’re often given by injection or IV, not as pills, because stomach acid would break them down. That’s why patients on biologics need regular doctor visits. The FDA approval, the process by which U.S. regulators evaluate biologics for safety, purity, and potency before they reach patients is stricter than for regular drugs. Manufacturing changes—even small ones—can affect how the drug works. That’s why companies must notify the FDA before altering production methods, and why some patients react differently when switched to a biosimilar.
Biologic drugs changed how we treat chronic illnesses, but they also opened up big questions about cost, access, and safety. Europe adopted biosimilars faster than the U.S., leading to lower prices and wider use. The U.S. is catching up, thanks to new rules in 2024 that make it easier for biosimilars to enter the market. But hospitals still hesitate—switching from one biologic to another can cause unpredictable side effects, even if regulators say they’re equivalent. And while biosimilars save money, the original biologics still dominate prescriptions because doctors are cautious. Patients should know: just because a drug is newer or cheaper doesn’t mean it’s better for them. What works for someone else might not work for you.
Behind every biologic drug is a story of science, regulation, and real-world trade-offs. The posts below cover exactly that: how these drugs are made, how regulators watch them, how they interact with other medications, and why switching to a biosimilar isn’t as simple as swapping one pill for another. You’ll find guides on manufacturing rules, legal risks for doctors, and how Europe and the U.S. handle these drugs differently. Whether you’re a patient, caregiver, or healthcare worker, this collection gives you the facts you need—not the marketing.
Biologic drugs are made from living cells, not chemicals, making them impossible to copy exactly. That’s why biosimilars aren’t generics - they’re highly similar versions that still require complex manufacturing and rigorous testing.