Triptans are effective for migraines but come with serious interactions and limitations. Learn who should avoid them, why they sometimes fail, and what to do when they don't work.
Triptan Contraindications: What You Must Know Before Taking These Migraine Drugs
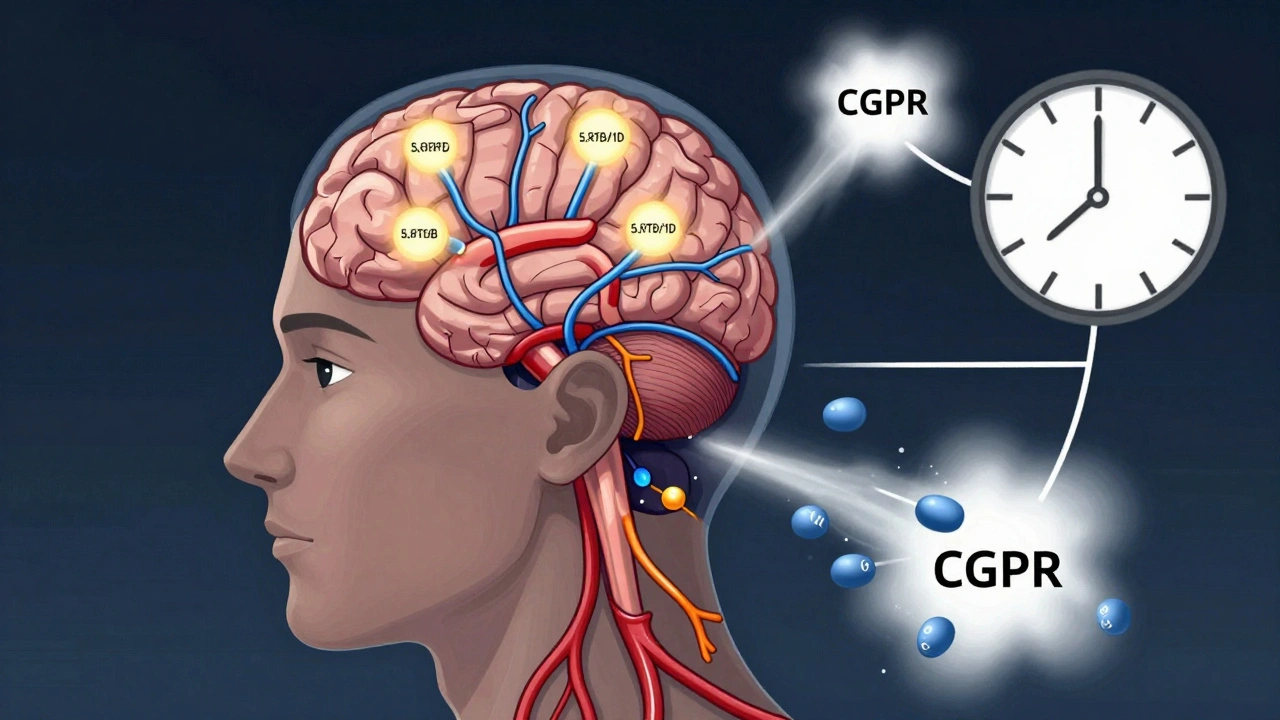
When you’re in the middle of a migraine, a triptan, a class of prescription drugs designed to stop migraine attacks by narrowing blood vessels in the brain and blocking pain pathways. Also known as serotonin receptor agonists, they’re one of the most targeted treatments for moderate to severe migraines. But they’re not safe for everyone. Taking a triptan when you have certain health conditions can lead to serious, even life-threatening reactions. That’s why knowing the triptan contraindications isn’t just good advice—it’s essential.
One of the biggest dangers is cardiovascular disease, a group of conditions affecting the heart and blood vessels, including past heart attacks, angina, or uncontrolled high blood pressure. Triptans constrict blood vessels, which sounds helpful for a headache—but if your arteries are already narrowed or damaged, that constriction can trigger a heart attack or stroke. People with a history of these issues are told to avoid triptans completely. Even if you’ve never had a heart problem, if you’re over 40 and have risk factors like smoking, diabetes, or high cholesterol, your doctor should check your heart health before prescribing one.
Another hidden risk is serotonin syndrome, a dangerous buildup of serotonin in the body that can cause fever, rapid heartbeat, confusion, and muscle rigidity. This happens when triptans are taken with other drugs that raise serotonin levels—like SSRIs, SNRIs, or even certain herbal supplements like St. John’s wort. Many people don’t realize their antidepressant and migraine med can clash. It’s not rare. Emergency rooms see cases every month. If you’re on any mental health medication, tell your doctor before starting a triptan.
There are other red flags too. Triptans aren’t safe if you’ve had a stroke or transient ischemic attack (TIA). They’re also not recommended for people with severe liver disease, because the body can’t break them down properly. And if you’ve had an allergic reaction to any triptan before, you shouldn’t take another—cross-reactivity is common. Even something as simple as taking two different triptans in the same day can be dangerous. These aren’t over-the-counter painkillers. They’re targeted drugs with narrow safety windows.
What’s surprising is how often these risks get overlooked. Patients are given a script and told to take it when the headache hits—no warning about heart risks, no checklist of what else they’re taking. That’s why understanding your own health history matters more than the brand name on the bottle. If you’ve ever had chest pain, high blood pressure, or are on antidepressants, you need to ask the right questions before you pop that pill.
Below, you’ll find real-world posts that dig into the hidden dangers, regulatory blind spots, and practical steps to stay safe. Some explain how insurance rules can force you into risky choices. Others show how pharmacies miss critical drug interactions. You’ll see what the FDA has flagged, how patients have been harmed, and what you can do to protect yourself. This isn’t theoretical. These are the mistakes people make every day—and the fixes that actually work.