Triptans are effective for migraines but come with serious interactions and limitations. Learn who should avoid them, why they sometimes fail, and what to do when they don't work.
Migraine Meds: What Works, What Doesn't, and How to Find the Right One
When you're stuck in a dark room with a pounding headache, migraine meds, medications designed to stop or prevent severe, recurring headaches often accompanied by nausea and sensitivity to light. Also known as headache medications, they're not just painkillers — they're targeted tools that act on specific nerve pathways in the brain. Not all headaches are the same. A tension headache feels like a tight band around your head. A cluster headache hits like a drill behind one eye. But a migraine? It’s a full-body event — light hurts, sound screams, and even walking can make it worse. That’s why regular ibuprofen often fails, and why knowing the right migraine meds can change your life.
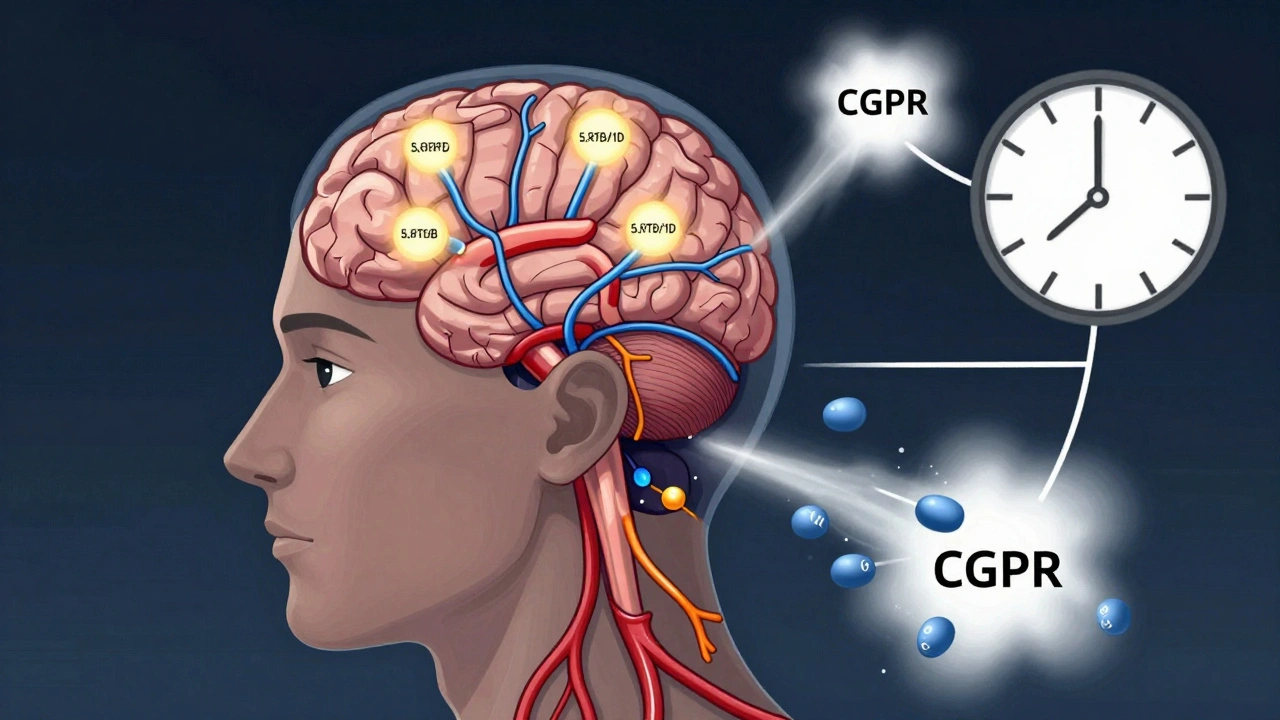
There are two main kinds: acute meds that stop an attack in progress, and preventive meds that reduce how often they happen. Acute options include triptans, a class of drugs that narrow blood vessels in the brain and block pain signals, commonly used during active migraine attacks, like sumatriptan or rizatriptan. These aren’t OTC — you need a prescription — but they work fast, often in under an hour. If triptans don’t help or cause side effects, newer options like gepants (ubrogepant, rimegepant) or ditans (lasmiditan) may be better. They target different receptors, so they’re safer for people with heart issues. Preventive meds are for those who get migraines more than four times a month. These include blood pressure pills like propranolol, antidepressants like amitriptyline, or even seizure drugs like topiramate. There’s also CGRP inhibitors — injectables like erenumab — that block a protein linked to migraine attacks. They’re expensive, but for some, they cut attacks in half.
What you don’t see on the label matters too. Insurance often forces you to try cheaper generics first — a rule called step therapy. That means you might be stuck on an old drug that doesn’t work while waiting for approval on something newer. And not all migraine meds play nice with others. Mixing them with certain antidepressants or painkillers can raise your risk of serious side effects. Even something as simple as skipping meals or sleeping too much can trigger an attack, no matter what meds you’re on. That’s why tracking your triggers — food, stress, weather, hormones — is just as important as the pill you take.
There’s no one-size-fits-all fix. What works for your friend might do nothing for you. And sometimes, the best option isn’t a pill at all — it’s a combination of meds, lifestyle tweaks, and knowing when to push back on your insurance. Below, you’ll find real-world insights on how these drugs actually perform, what the FDA says about their safety, how generics compare to brand names, and how to spot when a treatment isn’t just ineffective — it’s dangerous.