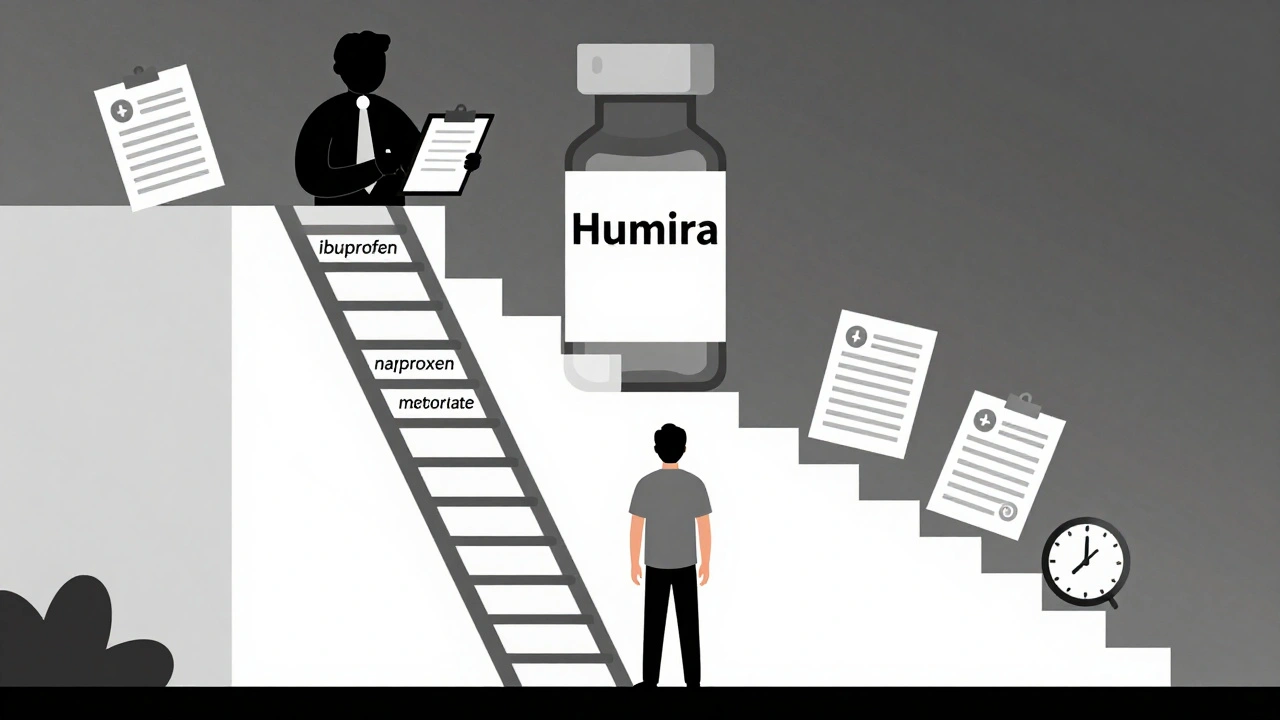
Step therapy forces patients to try cheaper generic drugs before insurers cover more expensive treatments. Learn how it works, when it fails, and what you can do to get exceptions quickly.
Fail-First Policy: What It Means for Your Medication Access
When your doctor prescribes a medication but your insurance says fail-first policy, a cost-control rule that requires patients to try cheaper or older drugs before approving newer ones. Also known as step therapy, it’s a common practice in managed care plans that can delay or block access to the right treatment. This isn’t just paperwork—it’s a real barrier that can make your condition worse while you wait for approval.
The fail-first policy, a cost-control rule that requires patients to try cheaper or older drugs before approving newer ones. Also known as step therapy, it’s a common practice in managed care plans that can delay or block access to the right treatment. isn’t just about saving money—it’s about shifting risk from insurers to patients. You might be forced to try a generic blood pressure pill that doesn’t work, then a different one, before finally getting the one your doctor actually recommended. That process can take weeks. For someone with ankylosing spondylitis, postpartum thyroiditis, or chronic pain, those weeks mean more pain, more fatigue, and more risk of complications. Hospitals and pharmacies see this daily—when patients can’t get their meds on time, ER visits go up, and long-term health suffers.
This policy doesn’t exist in a vacuum. It’s tied to prior authorization, a system where insurers require approval before covering certain drugs, which often goes hand-in-hand with fail-first rules. It’s also connected to pharmacy benefits, the structure insurers use to manage drug costs through formularies and tiered pricing. These systems are designed to cut costs, but they don’t always account for individual health needs. A patient with kidney issues might not tolerate the first drug on the list. Someone with depression might need a specific antidepressant that doesn’t interact with their other meds. The system doesn’t ask—it just pushes you down a checklist.
What you’ll find in the posts below are real stories and data about how these rules play out. You’ll see how fail-first policy affects people taking heart meds, biologics, and even over-the-counter supplements. You’ll learn how hospitals choose generics, how insurance forms decide what’s "first," and how patients fight back. Some posts show how patient counseling catches errors before they happen. Others reveal how supply chain issues make even approved drugs hard to get. This isn’t theory—it’s what’s happening in pharmacies, clinics, and homes across the country.