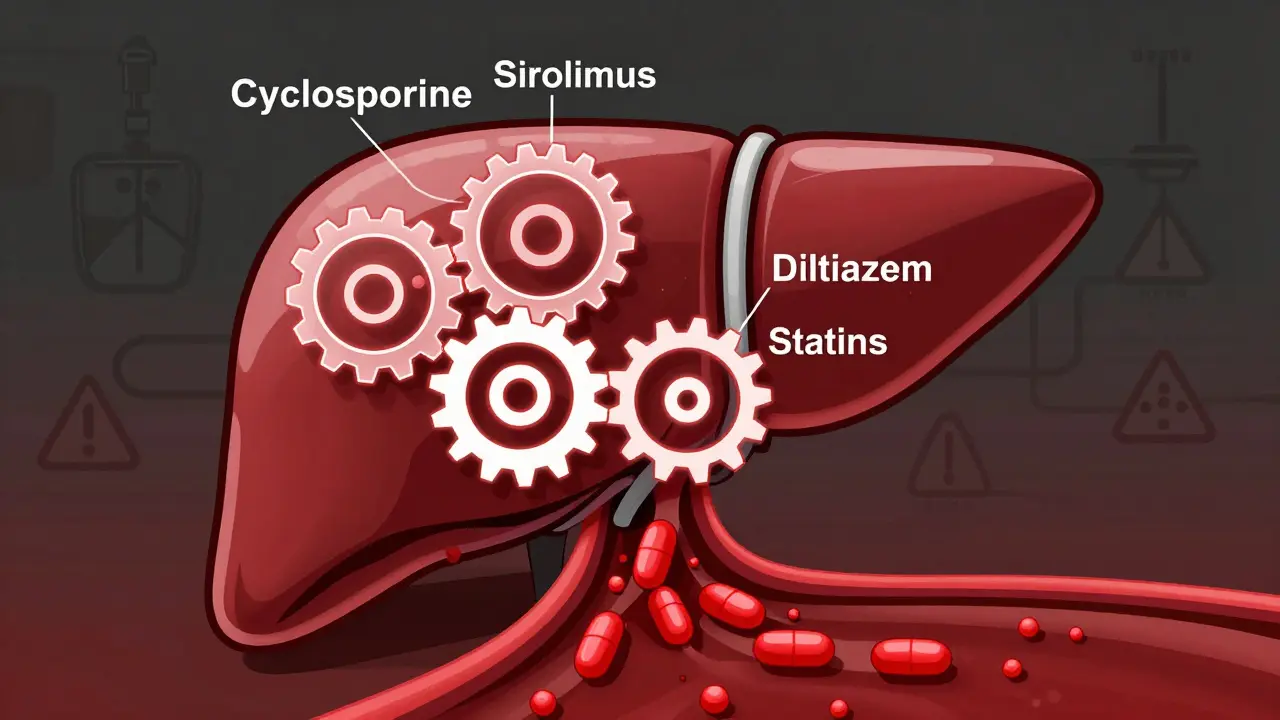
Cyclosporine inhibits the CYP3A4 enzyme, altering how your body processes many common drugs. This can lead to dangerous toxicity or transplant rejection. Learn which medications to avoid and how to stay safe.
Drug Interactions: How to Spot Risks and Stay Safe
One pill can change how another drug works — and not always for the better. Drug interactions happen when two medicines, a medicine and food, alcohol, or a supplement affect each other. Some are mild; others can be dangerous. Knowing the usual troublemakers helps you avoid real harm.
Common risky combinations you should know
Warfarin (a blood thinner) + NSAIDs (like ibuprofen) raises bleeding risk. Metronidazole (Flagyl) + alcohol can cause nausea, flushing, and a fast heartbeat — that’s why many guides tell you to avoid booze while on Flagyl. Grapefruit juice can boost levels of some statins and calcium-channel blockers, increasing side effects. Mixing SSRIs (antidepressants) with certain migraine drugs or other serotonergic meds can lead to serotonin syndrome — look for high fever, agitation, or muscle stiffness. Herbs and supplements aren’t harmless: St. John's wort lowers levels of many drugs, and valerian can add drowsiness when taken with sedatives.
How to check and avoid interactions — simple steps
Keep a single, up-to-date list of everything you take (prescription, OTC, vitamins, herbs). Share it with every prescriber and pharmacist. Read labels and the patient leaflet before starting a new drug. Use a reliable interaction checker (Drugs.com, PharmacyChecker, or ask your pharmacist) — they flag common issues fast. If you buy meds online, pick trusted pharmacies and confirm the active ingredient and dose; shady sites may sell wrong or counterfeit products that increase interaction risk.
Adjustments often fix interaction risks: timing doses (some drugs are safer taken hours apart), dose changes, or choosing an alternative medicine. For drugs cleared by the kidneys, like some seizure meds, kidney disease changes dosing — that’s why lab monitoring matters. If a health condition affects drug clearance (liver or kidney problems), talk to a clinician before adding anything new.
Watch for red flags: sudden severe headache, unexplained bleeding or bruising, high fever with muscle stiffness, fainting, or breathing trouble. These need urgent attention. Mild nausea, dizziness, or extra drowsiness still matter — they can signal an interaction that needs fixing.
Want practical help? Ask your pharmacist for a quick interaction check when you pick up prescriptions. Use DoctorSolve.com articles for plain-language guides on specific meds and interactions, but treat site info as a starting point — always confirm with a professional. A short conversation with your doctor or pharmacist can prevent a dangerous mix-up.
Small steps — one accurate meds list, a quick check, and asking the right questions — cut most interaction risks. Stay curious, stay cautious, and get help if anything feels off.
Pomegranate juice doesn't interact with medications the way grapefruit juice does. Human studies show no clinically significant effects on drug metabolism, despite early lab results suggesting otherwise. You can safely drink it with most meds.
Coordinating multiple prescriptions reduces dangerous drug interactions, prevents hospitalizations, and improves daily life. Use one pharmacy, a pill organizer, and medication synchronization to stay safe and in control.