Fiber & Hydration Calculator for Hemorrhoid Relief
Personalized Nutrition Calculator
Your Recommendations
RecommendedRecommended fiber intake: g/day
Recommended water intake: L/day
Current fiber intake: g/day |
Water intake should be in addition to fluids from food.
Why This Matters for Hemorrhoids
Aim for 25-30 grams of fiber daily as recommended in the article. This softens stool and reduces straining during bowel movements, which helps prevent hemorrhoids and anal itching.
Fiber also supports healthy digestion and prevents constipation, a major trigger for both conditions.
Ever notice that a painful lump in the rectum often comes with an annoying urge to scratch? You’re not alone. Many people experience both hemorrhoids and anal itching at the same time, and the two problems usually feed each other. This article breaks down why they’re connected, what triggers each condition, and practical steps you can take to stop the cycle.
Key Takeaways
- Hemorrhoids and anal itching share common causes like constipation, straining, and skin irritation.
- Internal and external hemorrhoids affect the body differently, but both can lead to itching.
- Simple lifestyle tweaks-more fiber, water, and gentle hygiene-often relieve both issues.
- If home care doesn’t help, over‑the‑counter creams or a visit to a proctologist may be needed.
- Preventing one condition usually prevents the other.
What Exactly Are Hemorrhoids?
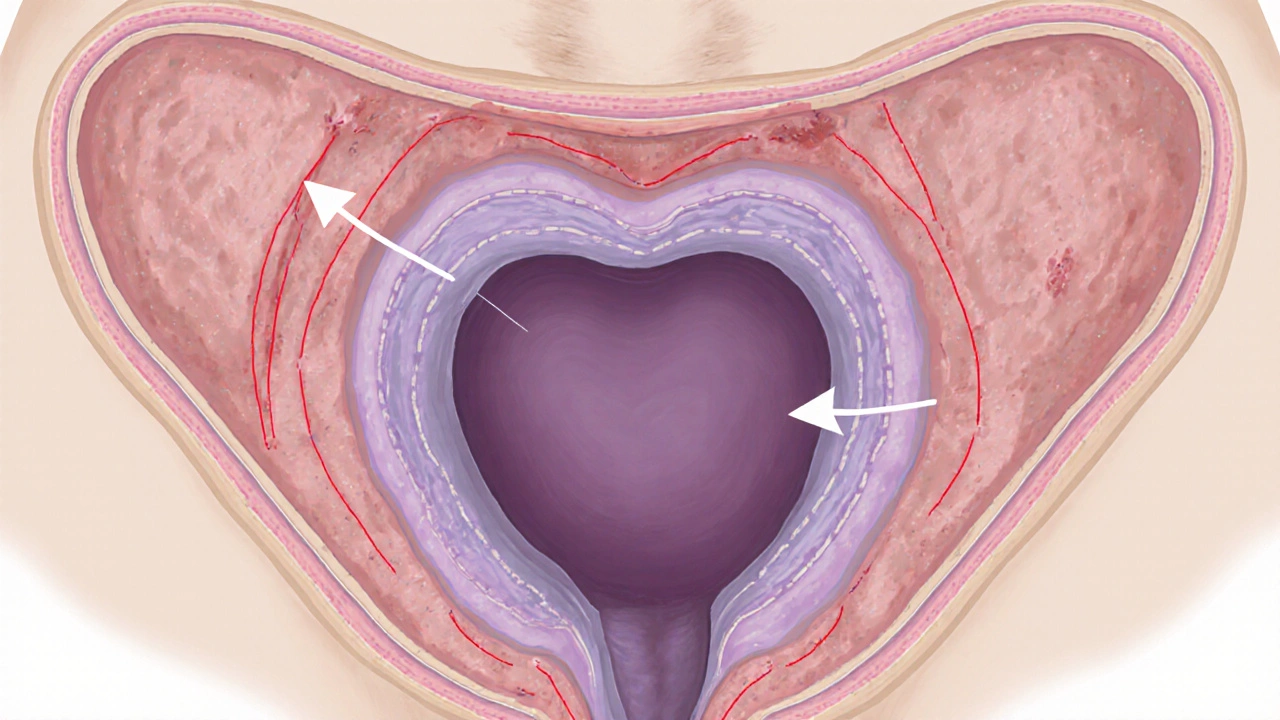
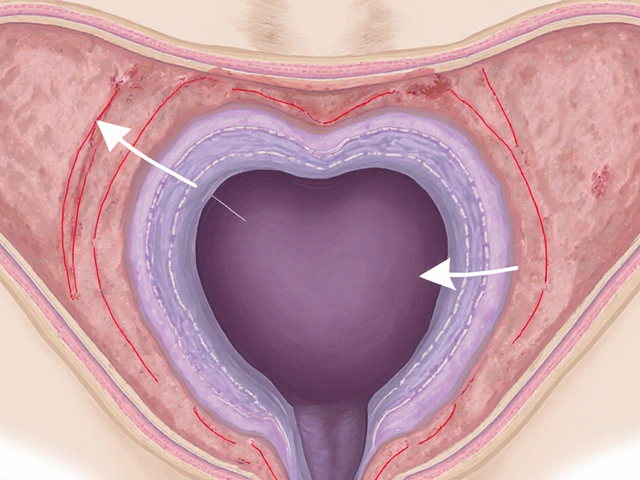
Hemorrhoids are swollen veins in the lower rectum or anus that can become inflamed, bleed, or prolapse. They’re similar to varicose veins you might see on a leg, but they sit in a much more sensitive area. Hemorrhoids are classified by where they develop and how severe they are:
- Internal hemorrhoids: located inside the rectum, usually painless until they prolapse.
- External hemorrhoids: sit just under the skin around the anus and often cause sharp pain or a hard lump.
- Grades I‑IV describe how far an internal hemorrhoid has prolapsed, with Grade IV staying outside permanently.
Although most people experience mild symptoms, severe cases can lead to chronic bleeding or thrombosis (a blood clot inside the vein).
What Is Anal Itching (Pruritus Ani)?
Anal itching, medically known as pruritus ani, is an uncomfortable urge to scratch the skin around the anus. It can feel burning, tingling, or simply irritating, and the skin often becomes red or raw from repeated scratching.
Pruritus ani isn’t a disease itself; it’s a symptom that can arise from many sources, ranging from simple hygiene issues to underlying medical conditions.

How the Two Conditions Feed Each Other
At first glance hemorrhoids and anal itching seem like separate annoyances, but they share key risk factors that create a feedback loop:
- Constipation and straining: When you push hard to pass stool, the pressure expands hemorrhoidal veins. The same pressure stretches the sensitive skin, making it more prone to itching.
- Moisture and irritation: Blood or mucus from a bleeding hemorrhoid can keep the skin damp, a perfect recipe for itchiness.
- Inflammation: Swollen tissue releases inflammatory chemicals that trigger nerve endings, resulting in both pain and itch.
- Scratching: Rubbing the area to relieve itching can damage the thin skin covering external hemorrhoids, worsening swelling and pain.
Breaking any link in this chain helps stop both problems.
Common Triggers You Can Control
Understanding the everyday habits that trigger hemorrhoids and anal itching makes prevention much easier.
- Constipation is a major driver; it forces you to strain during bowel movements. Causes include low fiber intake, dehydration, and certain medications.
- Straining often results from sitting too long on the toilet or trying to force a bowel movement.
- Heavy or spicy foods can irritate the lining of the rectum, especially if you have a sensitive gut.
- Prolonged sitting, especially on hard surfaces, puts constant pressure on the perianal veins.
- Improper hygiene-using harsh soaps or wiping too vigorously-strips natural oils and leaves the skin raw.
Simple Lifestyle Tweaks That Work
Before reaching for creams, try these evidence‑backed habits. According to a 2023 gastroenterology review, most patients see significant improvement after two weeks of consistent changes.
- Boost dietary fiber: Aim for 25‑30grams per day from fruits, vegetables, whole grains, and legumes. Fiber softens stool and reduces the need to push.
- Stay hydrated: At least 2liters of water daily keeps stool moist and easier to pass.
- Timed bathroom breaks: When you feel the urge, go promptly-delaying can dry out stool and increase straining.
- Sitz baths: Soak the anal area in warm water for 10‑15minutes after bowel movements. Sitz bath therapy reduces swelling and eases itching.
- Gentle cleansing: Use plain water or a mild, fragrance‑free cleanser. Pat dry with a soft towel; avoid rubbing.
- Exercise: Walking 30minutes a day promotes regular bowel movements and reduces pressure on the veins.
When Home Care Isn’t Enough: Medical Options
If symptoms persist after a couple of weeks, it’s time to consider over‑the‑counter (OTC) or prescription treatments.
| Category | Typical Ingredients | How It Helps | When to Use |
|---|---|---|---|
| Topical creams (OTC) | Hydrocortisone, witch hazel, lidocaine | Reduces inflammation, numbs pain, soothes itch | Mild to moderate symptoms |
| Suppositories (OTC) | Phenylephrine, zinc oxide | Constricts swollen veins, protects skin | Internal hemorrhoids, occasional bleeding |
| Prescription ointments | Stronger steroids or nitroglycerin | Targets severe inflammation or thrombosed hemorrhoids | Persistent pain, grade III‑IV prolapse |
| Oral pain relievers | Ibuprofen, acetaminophen | Alleviates pain and inflammation systemically | When topical options don’t control pain |
Always read the label for usage limits-excessive steroid creams can thin the skin further.
For chronic or severe cases, a proctologist (a specialist in the colon, rectum, and anus) can evaluate the need for procedures such as rubber‑band ligation, infrared coagulation, or, in rare cases, surgical removal.

What to Expect from Professional Treatments
Most minimally invasive procedures are done in a doctor’s office with little to no downtime. Rubber‑band ligation, for example, snaps the blood supply to an internal hemorrhoid, causing it to shrink within days. Recovery typically involves a few days of mild discomfort and a return to normal diet.
Surgical options like hemorrhoidectomy are reserved for giant or thrombosed hemorrhoids that don’t respond to other measures. Recovery can take 2‑3 weeks, and post‑op care focuses heavily on keeping the area clean and moist.
Quick Checklist to Stop the Cycle
- Increase fiber to 25‑30g daily (fruits, veggies, whole grains).
- Drink at least 2L of water each day.
- Schedule a 10‑minute Sitz bath after each bowel movement.
- Use gentle, fragrance‑free cleansing; pat dry.
- Apply an OTC cream with hydrocortisone for itch, but limit to 7days.
- If bleeding, pain, or swelling persists beyond 2weeks, book a visit with a proctologist.
Frequently Asked Questions
Can hemorrhoids cause permanent anal itching?
If the underlying cause (like chronic constipation) isn’t addressed, the itching can become a recurring problem. However, once the hemorrhoid heals and lifestyle changes are made, the itch usually resolves.
Is it safe to use hydrocortisone creams daily?
Short‑term use (up to 7days) is generally safe for mild itching. Prolonged use can thin the skin and increase the risk of infection, so follow package directions or ask a pharmacist.
Do I need to see a doctor if I only have itching?
If the itch is occasional and you have no bleeding, pain, or visible lumps, try the home‑care steps first. If it lasts more than two weeks or worsens, schedule a check‑up to rule out hemorrhoids, fissures, or infections.
Can diet alone cure hemorrhoids?
A high‑fiber, well‑hydrated diet can shrink many early‑stage hemorrhoids and prevent new ones. Severe cases may still need medical treatment, but diet is the foundation of any lasting solution.
What’s the difference between a hemorrhoid and an anal fissure?
A hemorrhoid is a swollen vein; an anal fissure is a tiny tear in the lining of the anus. Both can cause bleeding and discomfort, but fissures are usually more painful during bowel movements and heal slower.
Next Steps If You’re Still Unsure
Feeling stuck after trying the basics? Here’s how to move forward:
- Track your symptoms: Note when itching or pain occurs, what you ate, and bathroom habits. This diary helps a doctor pinpoint triggers.
- Consult a pharmacist: They can recommend the most appropriate OTC cream based on severity.
- Schedule a proctology appointment: Bring your symptom log. The specialist may perform a quick visual exam or recommend a minimal procedure.
Remember, most people find relief with simple changes. The key is to break the itch‑pain‑strain loop early, before the problem escalates.

Tom Smith
October 11, 2025 at 23:58So you’ve discovered that fiber and water are the holy grail for hemorrhoids-who would have guessed? In all seriousness, boosting dietary fiber to 25‑30 grams a day is a solid first step, and staying hydrated keeps the stool soft. Pair that with a gentle sitz bath after each bowel movement and you’ll likely see a reduction in both swelling and itch. Remember, the “no‑pain‑no‑gain” mantra doesn’t apply here; you’re actually trying to avoid pain. If you can manage this routine without turning your bathroom into a spa, you’re already ahead of the curve.
Kyah Chan
October 21, 2025 at 17:58It is incumbent upon the reader to recognize the interdependence of vascular engorgement and pruritic sensations as elucidated in the foregoing exposition. The author’s delineation of etiological factors such as constipation, straining, and moisture is commendably comprehensive. Nonetheless, the omission of a detailed discussion regarding the role of sphincter tone warrants critique. Moreover, the recommendation of over‑the‑counter corticosteroid preparations should be circumscribed by explicit contraindications. In sum, while the piece is largely informative, a more rigorous appraisal of pharmacologic adjuncts would enhance its scholarly merit.
Ira Andani Agustianingrum
October 31, 2025 at 10:58Hey there, friend! Let’s talk about making those tiny changes that add up big time. First off, grab a colorful bowl of mixed fruit or a handful of beans-those are fiber powerhouses that keep things moving. Then, keep a water bottle handy; sipping throughout the day is way easier than guzzling a gallon at once. Try a quick 10‑minute sitz bath after you’re done-trust me, it’s soothing and not as fancy as it sounds. If you can, stand up and stretch every hour; even a short walk can help the colon stay happy. Remember, the goal isn’t perfection, just consistency, and you’ll notice the itch and pain start to fade.
James Higdon
November 10, 2025 at 04:58It is a moral imperative that individuals assume responsibility for their bodily health, rather than relying on external interventions as a default. The article rightly underscores lifestyle modifications, yet one must also consider the ethical dimensions of self‑care neglect. Ignoring simple measures such as adequate fiber intake or proper hygiene not only endangers the individual but also places an undue burden on the healthcare system. Therefore, each person ought to diligently apply the recommended practices before seeking medical remedies. Only through disciplined personal stewardship can we hope to alleviate both discomfort and societal costs.
Wanda Smith
November 19, 2025 at 22:58The veil of normalcy that shrouds our daily routines is, in fact, a meticulously engineered distraction, designed to keep the masses oblivious to systemic forces perpetuating discomfort. When you contemplate the persistent itch, consider the hidden agendas of corporations that profit from the very products that aggravate your condition-over‑processed foods, artificial additives, and a culture of sedentary living. The true cure lies not merely in fiber and water, but in awakening to the reality that our bodies are battlegrounds in a quiet war of control. Embrace the discomfort as a signal, question every recommendation, and seek sovereignty over your own physiology.
Bridget Jonesberg
November 29, 2025 at 16:58One must, with an air of dignified exasperation, observe the sheer theatricality inherent in the discourse surrounding perianal maladies. The juxtaposition of clinical terminology against the mundanity of daily habits creates a tableau worthy of scholarly analysis. While the author’s suggestions-fiber enrichment, hydration, and modest hydrotherapy-are undeniably sound, they are presented with a simplicity that borders on the banal. Indeed, the path to alleviation is paved with nuanced ritual, requiring a patient to engage in a daily choreography of diet, posture, and hygienic precision. It is, after all, a performance where the audience is none other than oneself, and the applause is a modest respite from itch.
Marvin Powers
December 9, 2025 at 10:58Alright, fellow sufferers, let’s break down this whole hemorrhoid‑and‑itch saga with a mix of optimism and a dash of sarcasm, because life’s too short to be serious about a sore behind. First, kudos on even reading this far-most people would rather binge‑watch cat videos than confront the realities of anal discomfort. Second, the science is simple: fiber is your friend, water is your sidekick, and a sitz bath is the unlikely hero that swoops in to save the day. Third, you don’t need a PhD in gastroenterology to know that sitting on the throne for hours like it’s a throne room ceremony only amplifies the problem. Fourth, if you’re already making food choices that look like a cartoon junk food platter, expect the veins to throw a tantrum. Fifth, swapping that soda for a glass of water isn’t just trendy, it’s practically a sacrament in the temple of bowel health. Sixth, a daily walk-yes, even a 10‑minute stroll-stimulates peristalsis better than any miracle cream you can buy online. Seventh, gentle cleansing with warm water rather than harsh soaps preserves the natural barrier that keeps itching at bay. Eighth, if you must use a cream, pick one with hydrocortisone and limit it to a week; overuse turns your skin into a paper‑thin membrane prone to infection. Ninth, the moment you notice blood, don’t play the hero-schedule a proctologist visit before the drama escalates. Tenth, remember that “pain is weakness leaving the body” is a busted meme; listen to your body and give it the care it craves. Eleventh, keep a symptom diary; writing down what you ate, how often you went, and how you felt creates a roadmap for both you and your doctor. Twelfth, if you’ve tried everything and still suffer, don’t despair; modern medicine offers minimally invasive procedures that can resolve the issue without a week of bed rest. Thirteenth, celebrate every small victory-whether it’s a day without itching or a painless bowel movement. Fourteenth, avoid the temptation to compare your experience to internet anecdotes; each body is unique, and your journey is yours alone. Fifteenth, stay hopeful, stay consistent, and most importantly, stay kind to yourself-your backside will thank you. Finally, if anyone tells you that “it’s just a part of growing up,” politely remind them that adults have rights to comfort too.
Jaime Torres
December 19, 2025 at 04:58Fiber and water work.
Wayne Adler
December 28, 2025 at 22:58i hear ya man but real talk you cant just gulp water and hope magic happen, you gotta stick to a schedule & watch ur diet also sitz bath is cool but dont overdo it or ur skin gonna get raw i feel u
Shane Hall
January 7, 2026 at 16:58What you described is exactly the kind of compassionate guidance we need-think of your gut as a stage where every fiber‑rich bite and gentle splash of water cues a standing ovation of relief. By committing to those small, consistent habits you’ll script a narrative where the itch and pain become merely footnotes in your health story. Keep a journal, celebrate each painless trip to the bathroom, and remember that you’re the director of this production; the curtain will rise on comfort if you stay diligent.
Christopher Montenegro
January 17, 2026 at 10:58From a pathophysiological perspective, the author’s recommendations suffer from a paucity of mechanistic elucidation, thereby rendering the guidance suboptimal for clinical implementation. The omission of evidence‑based quantification of sphincter tonicity modulation constitutes a glaring methodological deficit. Moreover, the reliance on layman terminology obfuscates the requisite pharmacodynamic considerations inherent in corticosteroid topical administration. Consequently, the manuscript fails to meet the rigor expected of a peer‑reviewed compendium, and a comprehensive revision incorporating quantitative metrics is imperative.
Kyle Olsen
January 27, 2026 at 04:58It is evident, upon meticulous examination of the presented material, that the author has merely scratched the surface of a complex vascular pathology. One must consider, with due solemnity, the myriad of hemodynamic variables, including venous pressure gradients and collateral circulation, which are conspicuously absent from the discourse. The prevailing narrative, while serviceable for lay audiences, falls short of the scholarly gravitas demanded by seasoned clinicians. Thus, I implore the author to augment the treatise with a rigorous analysis befitting a professional treatise.
Sarah Kherbouche
February 5, 2026 at 22:58Honestly this whole thing sounds like another example of foreign health trends being pushed on us while we ignore good old American common sense. We got plenty of natural fiber in our diets if we just stop eating junk and start listening to real nutrition, not some overseas hype. The article could have just said “eat more veggies and drink water” without all the fancy fluff. Stop buying imported creams and trust what works here.