Cholesterol & Heart Disease Risk Calculator
Enter your information and click "Calculate Risk"
Understanding Your Results
- Low risk (<10%): Maintain healthy lifestyle
- Medium risk (10-20%): Consider lifestyle changes
- High risk (>20%): Discuss treatment options with your doctor
This tool uses the Framingham Risk Score to estimate your 10-year risk of developing cardiovascular disease. It considers age, gender, cholesterol levels, blood pressure, smoking status, and diabetes.
Note: This is a general tool and should not replace professional medical advice.
When doctors talk about heart attacks, they often point to a simple blood test: cholesterol. But why does a number on a lab report dictate the health of your arteries? This article untangles the chain of events that links high cholesterol to coronary artery disease (CAD) and gives you clear steps to break the cycle.
Quick Takeaways
- High LDL cholesterol drives plaque buildup inside coronary arteries.
- Atherosclerosis narrows vessels, leading to CAD symptoms or heart attacks.
- Lifestyle tweaks and statin therapy can reverse early damage.
- Regular screening catches problems before they become emergencies.
What Is High Cholesterol?
High cholesterol is a condition where the blood carries more lipids than the body needs, often measured as elevated low‑density lipoprotein (LDL) levels. LDL, sometimes called “bad cholesterol,” transports cholesterol from the liver to peripheral tissues. When too much LDL circulates, it can infiltrate arterial walls and start the plaque‑forming process.
High cholesterol can be genetic, diet‑related, or a by‑product of other health issues like diabetes. In most adults, it creeps up slowly, making routine blood work the only reliable way to spot it.
Understanding Coronary Artery Disease
Coronary artery disease (CAD) is the narrowing or blockage of the coronary arteries-the vessels that feed the heart muscle. The primary culprit behind CAD is atherosclerosis, a slow‑moving inflammatory process that turns cholesterol deposits into stubborn plaques.
When plaques grow large enough, they reduce blood flow, causing chest pain (angina), shortness of breath, or, in worst‑case scenarios, a heart attack.
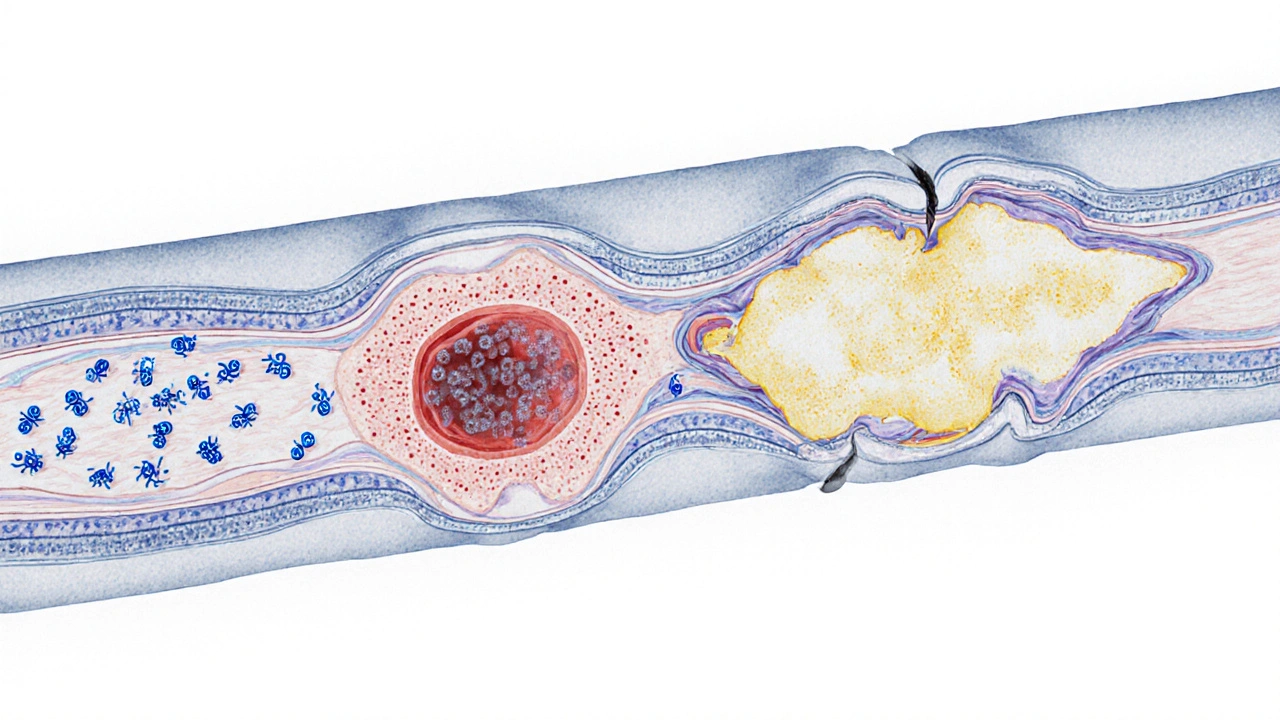
The Biological Link: From LDL to Plaque
At the heart of the connection lies the arterial wall. Here’s the step‑by‑step chain:
- LDL Penetration: Small LDL particles slip through the endothelial lining of an artery.
- Oxidation: Once inside, LDL oxidizes due to free radicals, turning into a form the immune system sees as foreign.
- Immune Response: Macrophages engulf oxidized LDL, becoming foam cells. Accumulated foam cells form the fatty streak, the earliest visible sign of atherosclerosis.
- Plaque Maturation: Smooth‑muscle cells migrate, calcium deposits form, and a fibrous cap develops over the fatty core.
- Rupture Risk: If the cap cracks, the clotting cascade triggers a thrombus that can completely block the artery, sparking a heart attack.
This cascade explains why even modest LDL elevations, when sustained over years, can set the stage for CAD.
How Other Lipids Play In
While LDL gets most of the blame, other blood lipids matter too:
| Marker | Ideal Range | Effect on CAD |
|---|---|---|
| LDL Cholesterol | <100 mg/dL | High levels accelerate plaque formation |
| HDL Cholesterol | >60 mg/dL | Helps clear cholesterol from arteries |
| Triglycerides | <150 mg/dL | Elevated levels worsen LDL oxidation |
| Lp(a) | <30 mg/dL | Genetic risk factor for atherosclerosis |
High‑density lipoprotein (HDL) acts like a garbage truck, ferrying excess cholesterol back to the liver for disposal. Low HDL, therefore, removes a natural brake on plaque buildup.
Assessing Your Personal Risk
A single cholesterol reading isn’t enough. Doctors look at the whole picture: age, family history, blood pressure, smoking status, and diabetes. The most common tool is the Framingham Risk Score, which estimates a 10‑year risk of a cardiovascular event.
If the score exceeds 10%, lifestyle changes and possibly medication become urgent.
Lifestyle Modifications That Lower LDL
Before reaching for pills, try these evidence‑based habits:
- Eat heart‑healthy fats: Swap saturated butter for olive oil or avocado; aim for at least two servings of fatty fish per week to boost omega‑3 intake.
- Increase soluble fiber: Oats, barley, beans, and apples bind cholesterol in the gut and pull it out of circulation.
- Exercise regularly: Moderate‑intensity aerobic activity (150min/week) can raise HDL by up to 10% and lower LDL by 5‑10%.
- Quit smoking: Smoking damages the endothelium, making LDL infiltration easier. Within a year of quitting, HDL improves noticeably.
- Maintain a healthy weight: Every 10% reduction in body weight can lower LDL by roughly 8%.
These steps are not just theory; multiple longitudinal studies (e.g., the Mediterranean Diet Trial, 2022) showed a 30% reduction in CAD events when participants followed similar regimens.
Medical Treatments: When Lifestyle Isn’t Enough
If your LDL stays above target after 3‑6 months of lifestyle work, doctors usually prescribe statins. Statins inhibit HMG‑CoA reductase, a liver enzyme that produces cholesterol, cutting LDL levels by 30‑50%.
Newer agents-PCSK9 inhibitors, ezetimibe, and bempedoic acid-offer alternatives for patients who can’t tolerate statins or need extra reduction.
Medication isn’t a magic wand. It works best alongside diet, exercise, and blood‑pressure control. A recent 2023 meta‑analysis found that combined therapy reduced major cardiovascular events by 25% compared to statins alone.
Monitoring Progress
After initiating any change, get a follow‑up lipid panel in 4‑12 weeks. Goal LDL for most high‑risk patients is <70mg/dL; for very high risk (e.g., previous heart attack), <55mg/dL is recommended.
Keep a log of your diet, activity, and any side effects. Sharing this with your clinician helps fine‑tune treatment.
Frequently Asked Questions
Can I have high cholesterol without developing CAD?
Yes. Genetics, overall inflammation, and protective factors like high HDL can keep plaque formation low even with borderline LDL. However, the risk rises the longer high LDL remains untreated.
Is fasting required for a cholesterol test?
Most modern labs accept a non‑fasting sample for LDL calculation, though triglyceride‑heavy meals can skew results. If your triglycerides are >400mg/dL, a fasting test is still advised.
Are natural supplements like red yeast rice as effective as statins?
Red yeast rice contains monacolin K, a compound chemically identical to low‑dose lovastatin. It can lower LDL by 10‑15%, but quality control varies, and it lacks the robust outcome data that statins have.
How quickly can lifestyle changes affect my LDL?
Significant reductions (5‑10%) can appear within 6‑12 weeks if you combine diet, exercise, and weight loss. Consistency is key; changes fade if habits slip.
What role does blood pressure play in CAD?
High blood pressure damages the arterial lining, making it easier for LDL to infiltrate. Managing hypertension alongside cholesterol offers a synergistic protection against atherosclerosis.
Putting It All Together
The link between high cholesterol and coronary artery disease isn’t a mystery-it’s a chain of biochemical events that you can interrupt. By knowing your numbers, adopting heart‑smart habits, and using medication when needed, you lower the odds of plaque‑induced blockages and keep your heart beating strong for decades.
Start today: schedule a lipid panel, swap one processed snack for a handful of nuts, and take a short walk after dinner. Small steps add up, and your arteries will thank you.



Dharmraj Kevat
October 1, 2025 at 15:08High cholesterol is the silent villain that seeps into artery walls and builds plaque that strangles the heart.
Lindy Fujimoto
October 7, 2025 at 13:08Behold the cascade of lipid chaos – an elegant ballet of LDL particles infiltrating the endothelium, oxidizing, and spawning foam‑filled lesions that masquerade as harmless deposits 🌪️💔. The mere mortal who ignores this molecular theatre invites catastrophe, for the arteries are not indifferent canvases but, rather, living galleries where every triglyceride stroke is judged by the relentless brush of time. 🍽️📉
darren coen
October 13, 2025 at 11:08Your cholesterol numbers are a mirror of lifestyle choices.
Jennifer Boyd
October 19, 2025 at 09:08Absolutely, think of each healthy bite as a heroic act against that relentless LDL tide – your heart will thank you, and the future you will be cheering from the sidelines! 🌟
Lauren DiSabato
October 25, 2025 at 07:08Frankly, the simplistic villain narrative masks the nuanced interplay of genetics, diet, and metabolic pathways; a reductionist view does little justice to the complex lipidomics at play.
Benjamin Herod
October 31, 2025 at 04:08While your critique is duly noted, the reality remains that without substantive intervention the silent accumulation proceeds unabated, rendering scholarly pontification moot.
luemba leonardo brás kali
November 6, 2025 at 02:08Indeed, cholesterol levels serve as a physiological ledger reflecting not only individual habits but also broader dietary customs; maintaining balance is a universally resonant pursuit.
Corey McGhie
November 12, 2025 at 00:08Oh, absolutely – because who wouldn't love a good cholesterol audit amid their curry night and weekend brunch? Yet, a dash of mindful choices can transform that ledger into a masterpiece.
Ajayi samson
November 17, 2025 at 22:08The reality is stark: most people drown in processed foods and ignore the warnings, choosing instant gratification over long‑term cardiac health, and the statistics scream that complacency is fatal.
Noah Bentley
November 23, 2025 at 20:08Let's not forget that “LDL” stands for “low‑density lipoprotein,” not “Lousy Daily Lament,” though your poetic lamentation might suggest otherwise.
Kathryn Jabek
November 29, 2025 at 18:08While your lexical jest oscillates between amusement and pedantry, the gravitas of hyperlipidemia demands a discourse that transcends facile wordplay, lest we trivialize a scourge that devours vitality with the elegance of a predator cloaked in academic veneer.
Ogah John
December 5, 2025 at 16:08One could argue that the very act of dissecting cholesterol's menace mirrors humanity's perpetual struggle to impose order upon chaos, a Sisyphean endeavor perpetually thwarted by our own appetites.
Kelvin Murigi
December 11, 2025 at 14:08Let’s cut through the philosophical haze and focus on actionable steps you can implement today to tame that rogue LDL. First, adopt a Mediterranean‑style diet rich in extra‑virgin olive oil, nuts, and fatty fish; studies consistently show a 30 % reduction in cardiac events for adherents. Second, incorporate at least 150 minutes of moderate aerobic exercise per week – a brisk walk, cycling, or swimming session will elevate HDL and lower LDL. Third, eliminate trans fats and dramatically reduce saturated fats; swap butter for avocado or nut butters, and choose lean protein sources. Fourth, increase soluble fiber intake through oats, barley, legumes, and apples; fiber binds cholesterol in the gut and escorts it out. Fifth, if you smoke, quit immediately – cessation improves endothelial function within weeks and raises HDL within months. Sixth, manage stress through mindfulness, yoga, or regular hobbies; chronic cortisol spikes can exacerbate lipid abnormalities. Seventh, monitor your numbers every three to six months; a baseline followed by periodic checks keeps you accountable. Eighth, if lifestyle changes alone fail to achieve target LDL (<100 mg/dL for most), discuss statin therapy with your clinician, acknowledging the modest risk of side effects versus the substantial benefit. Ninth, stay informed about newer agents like PCSK9 inhibitors if statins are insufficient or not tolerated. Tenth, maintain a healthy weight; shedding even 5‑10 % of body mass can lower LDL by up to 8 %. Eleventh, limit alcohol consumption to moderate levels – no more than one drink per day for women, two for men. Twelfth, prioritize sleep, aiming for seven to nine hours per night; poor sleep correlates with dyslipidemia. Thirteenth, involve your family; shared meals and joint activity reinforce adherence. Fourteenth, keep a food journal to identify hidden sources of cholesterol and sugars. Finally, remember that consistency beats intensity; sustainable habits forged over months will outlast any short‑term diet fad, ultimately preserving the vitality of your heart.