ADHD Medication Growth Tracker
Monitor Your Teen's Growth
Track height and weight measurements over time to detect potential medication side effects early.
Add Measurements
How to Interpret Results
This tool compares your measurements to CDC growth charts. A drop in height z-score by more than 0.5 or weight z-score by more than 1.0 within six months may indicate a concern. Consult your doctor if you see these patterns.
When a teenager starts taking ADHD medication, the goal is clear: focus improves, impulsivity drops, and school gets easier. But behind that progress lies a quiet concern many parents don’t talk about until it’s too late - growth. Not just in height, but in appetite, weight, and overall physical development. These aren’t rare side effects. They’re common. And they’re manageable - if you know what to watch for.
How ADHD Medications Work - and Why They Affect Growth
ADHD stimulants like methylphenidate (Ritalin, Concerta) and amphetamines (Adderall, Vyvanse) work by boosting dopamine and norepinephrine in the brain. These chemicals help with attention and self-control. But they also affect the body’s hunger signals and metabolism. That’s why appetite loss is one of the most frequent complaints. Studies show 50% to 80% of teens on these meds eat significantly less during the day. The medication hits hard in the morning, and by lunchtime, many feel no hunger at all.This isn’t just about skipping meals. It’s about calories. A 2023 survey on ADDitude Magazine’s parent forum found that 42% of teens on stimulants consumed fewer than 300 calories during school hours. That’s less than a single granola bar. By evening, when the drug wears off, they’re starving - and often overeat. One Reddit user shared: "My 14-year-old eats one snack at school, skips lunch, then eats enough for three people after 5 PM." This pattern can lead to poor nutrition, erratic weight gain, and long-term metabolic issues.
For growth, the impact is more subtle but just as real. Long-term studies, including the 2004 MTA follow-up and a 2014 analysis in the Journal of Child and Adolescent Psychopharmacology, show teens on stimulants for years grow about 0.5 to 1 inch (1.39-2.55 cm) shorter than expected. That’s not a lot - but it matters when your child is already on the lower end of the growth chart. The effect is strongest in the first 12 to 24 months. After that, growth often slows but doesn’t stop. Some catch up later. Others don’t.
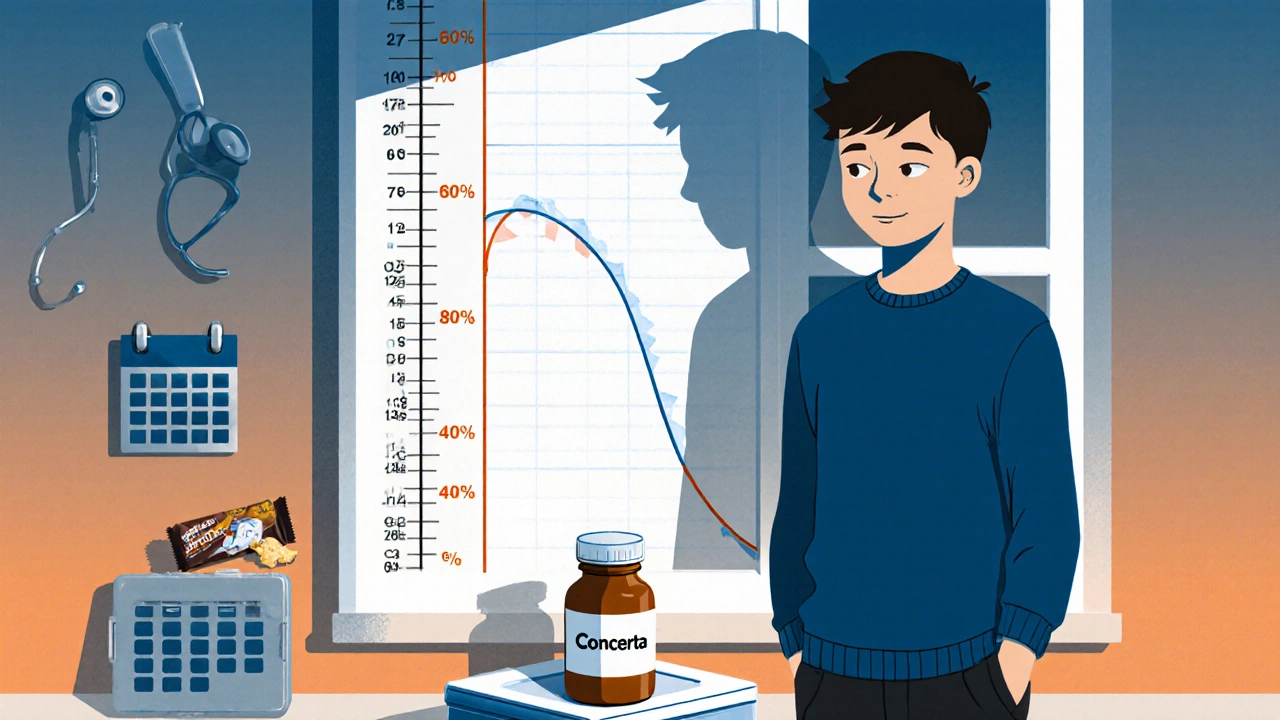
Stimulants vs. Non-Stimulants: The Growth Difference
Not all ADHD meds are the same when it comes to growth. Methylphenidate-based drugs like Concerta tend to have slightly less impact than amphetamine-based ones like Vyvanse. A 2019 meta-analysis in CNS Drugs found that after three years, teens on amphetamines were, on average, 1.7 cm shorter than their predicted height. Those on methylphenidate were 1.1 cm shorter.Non-stimulants like atomoxetine (Strattera) are different. They don’t suppress appetite as much and rarely affect growth. But here’s the trade-off: they’re 30% to 40% less effective at reducing core ADHD symptoms, according to the 2017 Cochrane Review. So if your teen struggles with focus and organization, switching to Strattera might mean more missed assignments and social friction.
There’s also a new option: Adhansia XR, an extended-release amphetamine approved by the FDA in 2023. Early trials showed 18% less weight loss compared to older formulations. That’s promising - but it’s not a cure. It’s just a small improvement.
Who’s Most at Risk?
Growth suppression doesn’t hit everyone the same way. Teens already in the lower percentiles for height or weight are more vulnerable. So are those on higher doses. A teen on 72 mg of Vyvanse is far more likely to see changes than one on 20 mg of methylphenidate.Family history matters too. If a parent was a late bloomer, the teen might just be genetically slower to grow - and the medication could be masking that. That’s why baseline measurements are critical. Before starting any medication, doctors should record height, weight, and BMI. Then track them every three months for the first year, and every six months after that - as recommended by the American Academy of Pediatrics.
If a teen’s height z-score drops by more than 0.5 or their weight z-score by more than 1.0 within six months, it’s time to act. That’s the threshold Cleveland Clinic uses. It’s not about being "underweight" - it’s about a sudden drop in growth speed. That’s the red flag.
Practical Strategies: Eating, Timing, and Breaks
You can’t just tell a teen to "eat more." Appetite suppression is biological, not behavioral. But you can work around it.- High-calorie breakfast before the med kicks in. Give them a smoothie with peanut butter, banana, oats, and whole milk at 6:30 AM. By 8 AM, when the drug starts working, they’ve already gotten 500+ calories.
- Snacks before lunch. Cheese sticks, trail mix, or a protein bar before school can help. Even if they don’t eat lunch, they’ve had something.
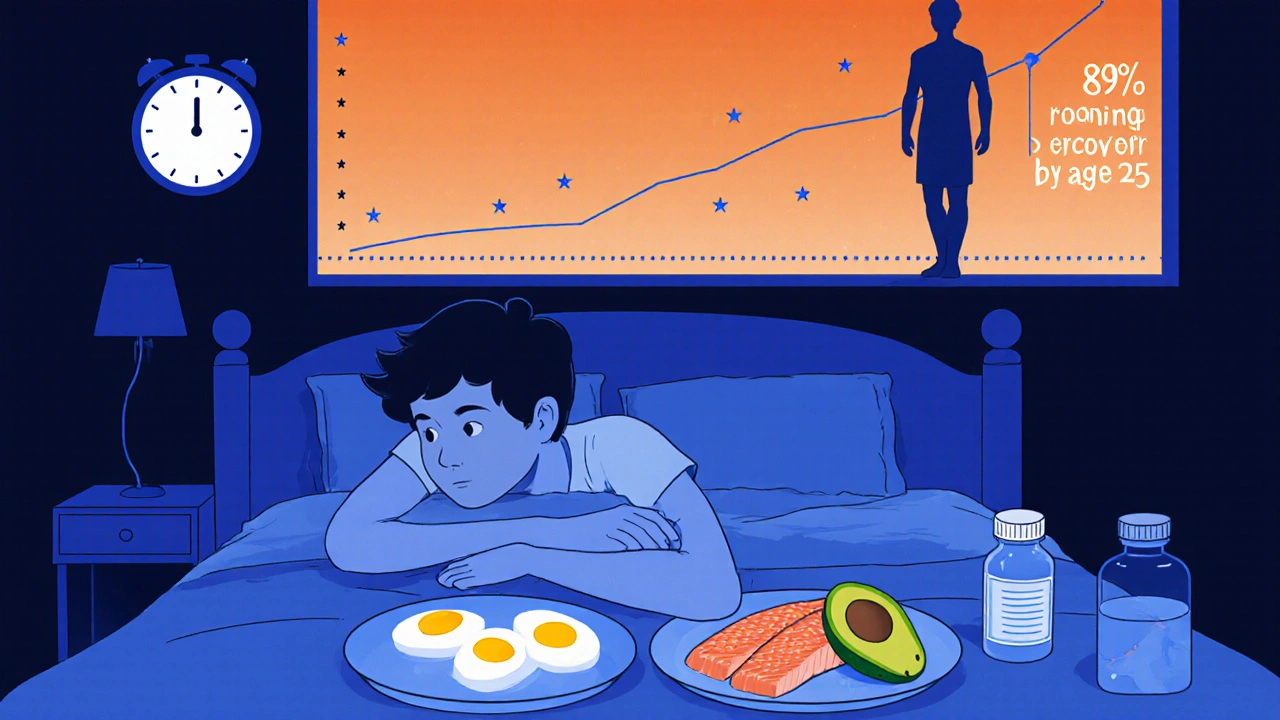
- Big, nutrient-dense dinners. After school, when the meds wear off, load the plate. Eggs, salmon, avocado, whole grains - focus on calories and protein, not just volume.
- Consider a weekend or summer "med holiday." The 2013 Journal of Pediatrics study found 87% of teens caught up 75% of their growth within six months of stopping meds. If your teen is stable academically and socially, a break during summer or holidays can help. About 73% of pediatric psychiatrists support this approach.
In extreme cases, doctors may prescribe cyproheptadine, an appetite stimulant. It’s not first-line - it’s used when weight loss hits 10% or more of body weight. One parent told CHADD: "After eight months on Concerta, my daughter dropped from the 50th to the 15th percentile. We switched to Strattera. She gained 12 pounds in three months."
What the Experts Say
There’s debate. Dr. Joseph Biederman from Harvard says the height loss is "clinically insignificant" compared to the benefits - better grades, fewer car accidents, lower risk of substance abuse. He’s right. ADHD meds save lives in the long run.But Dr. Glen Elliott from Children’s Health Council warns: "We can’t ignore dose-dependent suppression, especially in kids already struggling to grow." He’s also right. For some teens, that inch matters. It affects self-esteem. It affects clothing sizes. It affects how they see themselves.
The 2023 MTA follow-up study offers hope: 89% of teens who had growth delays caught up to their genetic potential by age 25. Only 11% ended up more than 1.5 cm shorter than expected. That’s a strong signal: most of the impact is temporary. But waiting until 25 to see results isn’t helpful for a 14-year-old who’s being teased for being "the smallest in class."
Monitoring Is Non-Negotiable
The FDA requires growth monitoring on stimulant labels since 2013. Yet, a 2021 AAP survey found only 92% of pediatric practices use electronic growth charts - meaning 8% still rely on paper logs or memory. That’s risky.Here’s what you need to do:
- Get baseline measurements before starting medication.
- Track height and weight every 3 months for the first year, then every 6 months.
- Plot them on a CDC growth chart - don’t just look at the numbers.
- If growth slows more than expected, talk to the doctor about dose reduction, timing changes, or switching meds.
- Don’t wait for weight loss to become severe. Catch it early.
Some clinics now use pharmacogenetic testing - like Genomind’s CYP2D6 test - to predict how a teen will metabolize stimulants. In their 2022 trial, 40% fewer growth-related side effects occurred when dosing was guided by genetics. It’s not standard yet, but it’s coming.
The Bigger Picture
ADHD medication use among U.S. adolescents has jumped from 76.5% in 2016 to 84.2% in 2022. Sales hit $17.2 billion globally in 2022. We’re treating more teens than ever. That’s progress - but it also means we need better monitoring.It’s not about avoiding meds. It’s about using them wisely. The goal isn’t just to quiet the symptoms. It’s to raise a healthy, confident teen who grows into a healthy adult. That means watching the scale, the height chart, the empty lunchbox, and the late-night binge. It means asking the hard questions: "Are we helping them now without hurting them later?"
There’s no perfect answer. But there is a careful path. Track. Adjust. Communicate. And never assume that because the ADHD is under control, the body is too.
Do ADHD medications permanently stunt growth?
No, not for most teens. Long-term studies show that 89% of adolescents who experienced growth suppression while on stimulants caught up to their genetic height potential by age 25. Only about 11% ended up more than 1.5 centimeters shorter than expected. The effect is usually temporary and most noticeable in the first one to two years of treatment.
How much weight loss is too much on ADHD meds?
Losing more than 10% of body weight in a short time is a red flag. That’s the threshold most pediatricians use to consider changing medication or adding an appetite stimulant. A drop in weight percentile - like going from the 50th to the 15th - is also a sign the current treatment isn’t working for their physical health.
Should I give my teen a break from ADHD meds?
A medication holiday - like stopping during summer break or weekends - can help with appetite and growth recovery. About 73% of pediatric psychiatrists support this approach, especially if the teen’s symptoms are manageable without daily meds. But don’t stop without talking to the doctor. Sudden discontinuation can cause rebound symptoms or mood swings.
Are non-stimulant ADHD meds better for growth?
Yes, non-stimulants like atomoxetine (Strattera) have minimal impact on appetite and growth. But they’re also 30% to 40% less effective at reducing core ADHD symptoms like inattention and impulsivity. They’re a good option for teens who struggle with weight loss or who don’t respond well to stimulants - but not a first choice if focus is severely impaired.
What should I feed my teen on ADHD medication?
Focus on calorie-dense, nutrient-rich foods eaten before the medication kicks in. Try high-calorie breakfasts (smoothies with peanut butter, whole milk, oats), cheese sticks, nuts, and avocado. Save larger meals for after school when the drug wears off. Avoid low-calorie snacks like fruit alone - pair them with protein or fat to boost calorie intake.
How often should my teen’s height and weight be checked?
The American Academy of Pediatrics recommends checking height and weight at baseline, then every 3 months during the first year of treatment, and every 6 months after that. If growth slows significantly, more frequent checks may be needed. Always use a CDC growth chart - don’t rely on memory or verbal reports.
What Comes Next
The National Institute of Mental Health is funding a $4.2 million study (2023-2026) to finally answer how long and how much ADHD meds affect growth. Meanwhile, the American Academy of Pediatrics is updating its guidelines in late 2024 to include clearer intervention thresholds.For now, the message is simple: monitor closely. Don’t assume growth will fix itself. Don’t wait for a crisis. Work with your doctor to balance symptom control with physical health. Because a teen who can focus in class but can’t fit into their jeans isn’t thriving - they’re just surviving.

Robert Merril
November 16, 2025 at 21:00So let me get this right we give kids amphetamines to help them sit still in class but now we’re surprised they stop growing like normal humans lmao
Also who the fuck writes 8000 words about a kid not eating lunch
Just feed em a peanut butter banana smoothie before school and call it a day
Noel Molina Mattinez
November 17, 2025 at 07:40My son on vyvanse lost 15lbs in 4 months and now he’s the smallest in his class and the other kids call him twig
I asked the doc to switch to strattera and they said no because his grades improved
So now he’s a ghost with a backpack and a 4.0 GPA
Roberta Colombin
November 18, 2025 at 01:01Thank you for writing this with such care and clarity.
As a parent of a child with ADHD, I want to say how much this helps.
Many of us are scared to speak up because we feel guilty for wanting our child to be healthy as well as successful.
But growth matters. Weight matters. Self-esteem matters.
We don’t have to choose between focus and being a whole person.
And we deserve better guidance from our medical system.
Thank you for reminding us we’re not alone.
Dave Feland
November 18, 2025 at 23:14Let’s be clear - this isn’t about growth suppression. It’s about the pharmaceutical industry’s calculated exploitation of neurodivergent children under the guise of ‘treatment.’
The MTA study? Funded by NIH with ties to Lundbeck and Shire.
The ‘catch-up’ by age 25? A statistical mirage - longitudinal data is cherry-picked to avoid liability.
And now they’re pushing pharmacogenetic testing to monetize even more testing - all while parents are told to ‘trust the science.’
Meanwhile, the FDA’s own labeling requires growth monitoring - but no mandatory reporting of long-term stunting.
This isn’t medicine. It’s a controlled experiment with a profit margin.
Ashley Unknown
November 20, 2025 at 09:09Okay so I just found out my daughter’s pediatrician didn’t even plot her growth on a chart for 11 months and now she’s dropped from the 65th to the 8th percentile and I’m crying in the car right now because I thought the meds were helping her but now I realize she’s been starving herself silently for a year and the school nurse said she’s always the last to eat lunch and I didn’t even know because she’s so quiet and now I’m wondering if she’s going to be permanently small and if she’ll ever feel like she belongs in her own body and why didn’t anyone tell me this was a thing and why is the system so broken and why do we have to fight so hard for our kids to just be okay and I hate that I didn’t see it sooner and I hate that I feel guilty and I hate that I have to choose between her focus and her future and I hate that I’m not the only one feeling this way and why is no one talking about this more
PLEASE SOMEONE TELL ME I’M NOT CRAZY
Georgia Green
November 20, 2025 at 20:54My kid on 30mg Concerta eats like a wolf after school - pasta, eggs, peanut butter sandwiches, whole milk.
Before meds? He’d pick at food.
After meds? He’s a beast at dinner.
Height chart? Still on the 40th percentile.
Just feed him before the drug hits and after it wears off.
It’s not magic. It’s timing.
And yes, we do a summer break.
He’s fine.
Christina Abellar
November 21, 2025 at 03:38Baseline measurements matter.
Track every 3 months.
Simple.
Do it.
Eva Vega
November 22, 2025 at 10:56From a clinical pharmacology standpoint, the pharmacokinetic variability of CYP2D6 polymorphisms significantly modulates the plasma concentration-time profiles of amphetamine derivatives, thereby influencing both therapeutic efficacy and somatic side effect burden - particularly in pediatric populations with high metabolic clearance phenotypes. This necessitates individualized titration protocols informed by genotypic stratification to mitigate growth-related adverse events, which are dose-dependent and temporally correlated with peak plasma concentrations during the circadian cycle.
Matt Wells
November 23, 2025 at 02:30It is regrettable that the article fails to adequately contextualize the statistical significance of the 1.5 cm growth discrepancy within the broader framework of population-based normative data. The effect size, while statistically detectable, remains clinically negligible when compared against the well-documented reduction in delinquency, substance abuse, and academic failure associated with stimulant therapy. To prioritize somatic metrics over functional outcomes is to misplace the therapeutic objective. The child who can read, write, and regulate emotion is far more likely to achieve autonomy and self-sufficiency - regardless of height percentile.